Confirmation
A02: Patient Assessment
Reviewed: December 2, 2020
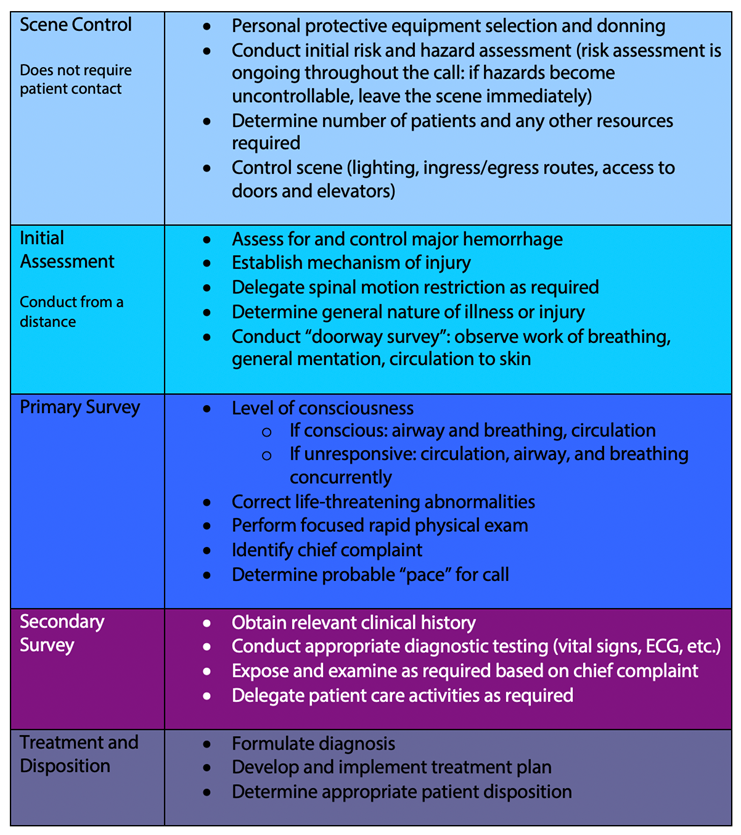
Essentials
- The goal of patient assessment is to construct a mental model of the clinical condition under consideration and to develop an effective and appropriate care plan in a safe and appropriate environment.
- Regardless of the specific model used, all patient assessments must include, at a minimum:
- A dynamic and ongoing risk assessment, both prior to and following contact with the patient.
- A preliminary examination, made from first visual contact, intended to gather information on potential life-threatening hemorrhage, mechanism of injury, and establish a general impression of overall clinical condition.
- A primary survey aimed at identifying life-threatening conditions to allow for prioritization of interventions.
- The identification of a chief complaint and its associated history.
- A clinical history of the patient, including current medications, any allergies, and current levels of intervention (as applicable).
- Focused physical and functional exams to include or exclude relevant differential diagnoses.
Scene Control and Hazard Assessment
The assessment process begins prior to making contact with the patient. The scene survey forms the basis of the ongoing risk assessment that continues throughout the entire call; paramedics and EMRs/FRs must be aware of hazards in the patient’s environment, including along the ingress and egress routes, and take appropriate steps to mitigate those hazards.
Guidance on managing specific hazards is outlined in the High Risk Hazard guide. In cases where hazards cannot be suitably controlled, or mitigation strategies are unclear, paramedics and EMRs/FRs should withdraw to a safe distance and seek additional resources. Withdrawing may be as simple as waiting in a hallway or involve leaving the scene completely and moving to a location that is known to be safe. Paramedics and EMRs/FRs must exercise judgment when deciding whether a scene is safe or not, and in all cases, err on the side of physical distance.
Control of the scene can be multifaceted. Wherever possible, lights on the ambulance should be used to illuminate paths to and from residences. Paramedics and EMRs/FRs must ensure a clear and direct route is continually available between the ambulance and the patient; doors should be left open, or at a minimum unlocked. When possible, uninvolved bystanders should be removed from the immediate area to protect the patient’s privacy, to ensure paramedic and EMR/FR safety, and to minimize distractions while managing the patient.
In all cases, paramedics and EMRs/FRs must ensure that roles and responsibilities are clearly defined. Paramedics and EMRs/FRs should be particularly diligent about discussing these when confronted with cases predicted to be complex for any reason and the precise nature of that complexity will vary from paramedic and EMR/FR to paramedic and EMR/FR. Collaborative assessments making effective use of the skills of all providers at a scene will improve patient care.
Initial and Primary Survey
A significant amount of information can be obtained 'from the doorway', prior to making physical contact with the patient. The goal of the initial survey is to identify life-threatening hemorrhage requiring immediate control, identify a potential mechanism of injury, delegate responsibilities for spinal motion restriction, and formulate a general impression of the patient’s overall condition. The overall impression can help paramedics and EMRs/FRs to establish priorities for care and to set the pace of the call; patients who appear unwell require more immediate assessment and intervention, while patients who appear well may benefit from a more relaxed tempo. Paramedics and EMRs/FRs should observe the patient’s work of breathing, the appearance of their skin, and their mentation to form a general impression of the patient's condition and acuity.
Prior to beginning a formal primary survey, life-threatening hemorrhage must be controlled. This can be accomplished through the use of delegated direct pressure or placement of a tourniquet as needed. See D02: Bleeding for additional details on hemorrhage control.
The primary survey is intended to guide paramedics and EMRs/FRs in the identification of other life-threatening problems. The assessment should begin with an evaluation of the patient’s level of consciousness using a coarse scale; patients will either be spontaneously alert, responsive to voice, responsive to pain, or unresponsive. If a pain stimulus is required, it should be appropriate for the diagnostic purpose: sternal rubs are generally unhelpful and should be avoided, while trap squeezes, supraorbital pressure, and fingernail pressure are more useful for establishing levels of consciousness and identifying focal neurological deficits.
In patients who are conscious, paramedics and EMRs/FRs should assess the airway, breathing, and circulation. Patients who are unconscious should have their circulation and breathing assessed simultaneously and chest compressions initiated if pulses are absent; formal assessment of the airway can be deferred until resuscitation is underway. In all cases, issues or problems identified in the primary survey must be managed immediately upon discovery, either directly by the attending paramedic or EMR/FR, or delegated as a task to other providers.
The primary survey should conclude with an evaluation of the patient’s skin colour and temperature followed by a rapid but comprehensive physical exam tailored to the overall clinical scenario.
Following the completion of a primary survey and its associated interventions, a chief complaint must be identified, and a history of the chief complaint obtained.
Secondary Survey
At this point, vital signs should be taken (ideally by delegation). Paramedics and EMRs/FRs may have gathered enough information at this point to formulate an appropriate treatment plan, or they may need to interview the patient and conduct a physical examination to gain further details. Interventions or investigations that are time-sensitive should be performed at this point, while preparations are being made for conveyance of the patient if that is the most appropriate disposition.
Clinical Scores and Assessment Tools
BC Emergency Health Services advocates the use of the National Early Warning Score 2 (NEWS2) to identify patients at risk of rapid deterioration. NEWS2 scores should be obtained on all patients and used to guide clinical decision-making, particularly in the areas of conveyance, destination or clinical pathway selection, pre-arrival notification, ongoing monitoring, and emergency department advocacy. Note: SpO2 Scale 1 is for patients not diagnosed with COPD; SpO2 Scale 2 is for patients diagnosed with COPD.
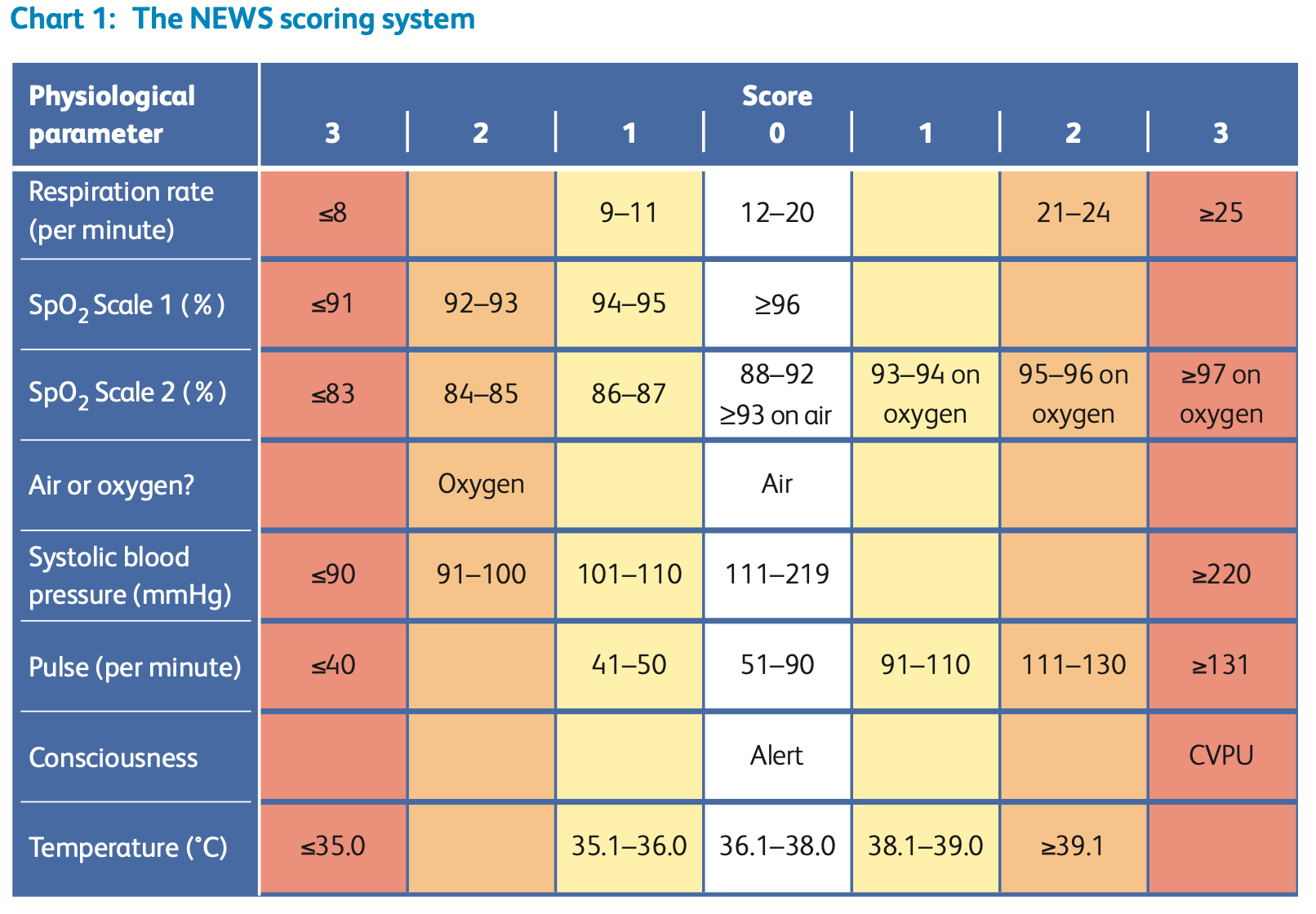
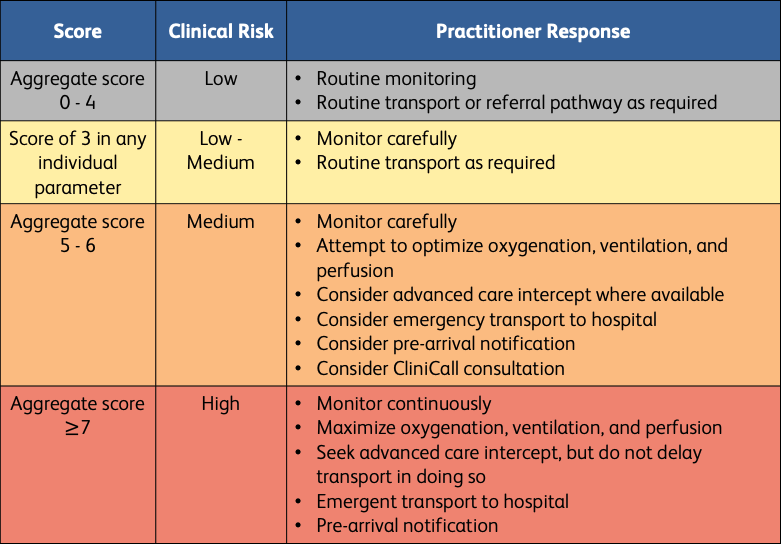
NEWS2 is not intended to replace sound clinical judgment. Its purpose is to alert practitioners to the risk of sudden deterioration and to help identify those patients who require more aggressive monitoring, treatment, and advocacy. This is particularly valuable in the context of infectious diseases and suspected sepsis.
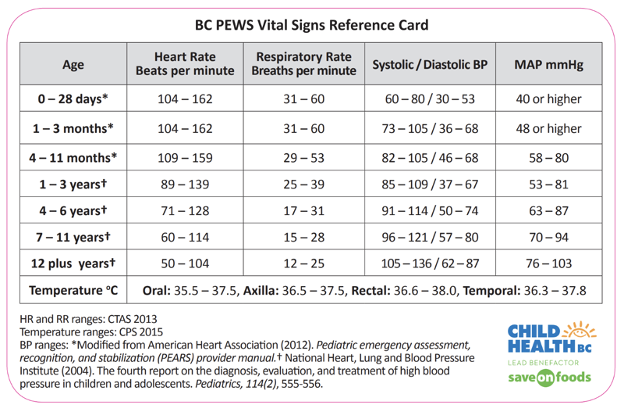
For pediatric patients, an equivalent scoring system -- the BC Pediatric Warning Score (PEWS) -- can be used for the same purposes as NEWS2.
Treatment and Disposition
Paramedics and EMRs/FRs must exercise judgment and manage their time on-scene effectively. Tasks that have minimal effects on clinical outcomes should be deferred until the patient is en route to the destination facility. On-scene tasks should be limited to those procedures and interventions that will yield meaningful information that affects the overall management plan or that addresses an immediate and urgent patient need. Attending paramedics and EMRs/FRs should not feel pressured to perform all tasks: the effective use of one’s partner and other responders is a hallmark of effective clinical practice and the delegation of tasks – obtaining vital signs, completing documentation, initiating vascular access – is critical to good time management while on-scene.