Confirmation
A03: Clinical Handover and Communication
Introduction
Effective communication during transitions of patient care from one health care provider to another, or handovers, is a critical component of a patient safety-centred culture. Ineffective handovers cause confusion and are the most common underlying cause of adverse patient events across health care, regardless of setting or the specific providers involved.
All health care professionals, including paramedics, emergency medical responders, first responders, nurses, and physicians have an obligation to ensure that patient information is appropriately and comprehensibly shared with other providers. A structured tool that promotes the use of a standardized handover format can significantly improve patient safety during critical phases of care, and encourages the development of a shared mental model that allows for more information sharing.
The ATMIST AMBO mnemonic tool is BCEHS’s approach to structured and standardized handovers during most clinical scenarios. A separate tool, SBAR, is intended for use during clinical consultations (i.e., with CliniCall or EPOS). All providers, regardless of licensure or role, are expected to use the ATMIST AMBO tool for all transitions of care, both in- and out-of-hospital. The use of a structured handover tool is a required organizational practice for accreditation, highlighting its importance to strengthening patient safety.
Essentials:
To effectively perform a clinical handover, paramedics, emergency medical responders, and first responders should:
- Ensure an appropriate environment for handover with consideration for patient confidentiality and to limit non-critical interruptions during the handover.
- Provide relevant, timely, accurate information in common language without the use of abbreviations or jargon.
- Use a structured, standardized tool to provide this information.
Clinical handovers of critical patients should, ideally, include a 20-30 second period where the patient remains on the ambulance stretcher, with the receiving providers in a “hands off, eyes on” period while the structured handover is completed. The goal of this period is to minimize distractions during the handover, allowing providers to exchange information without having to compete with external tasks, conversation, or instructions, and to increase overall team situational awareness. Patient condition may not always permit this 20-30 second pause, however all providers must, while giving or receiving a handover report, focus directly on the handover itself rather than attending to additional patient care tasks.
General
A structured clinical handover tool is designed to provide a mechanism to consistently provide patient information during a transition of care. Structured tools work because they provide a standardized framework for the presentation and communication of relevant clinical data, formatting and organizing information in such a way as both the sending and the receiving providers know what to expect at each step of the handover. This standardized format speeds the creation of a shared mental model and reduces the chances that important information is accidentally missed or excluded in handover conversations.
British Columbia paramedics, emergency medical responders, and first responders use two handover tools: ATMIST AMBO and SBAR. Both reduce adverse events and improve the accuracy of information exchange, although they serve different roles. Providers working in the out-of-hospital care system in British Columbia must become familiar with these tools, and use them consistently while engaged in patient care activities.
ATMIST AMBO
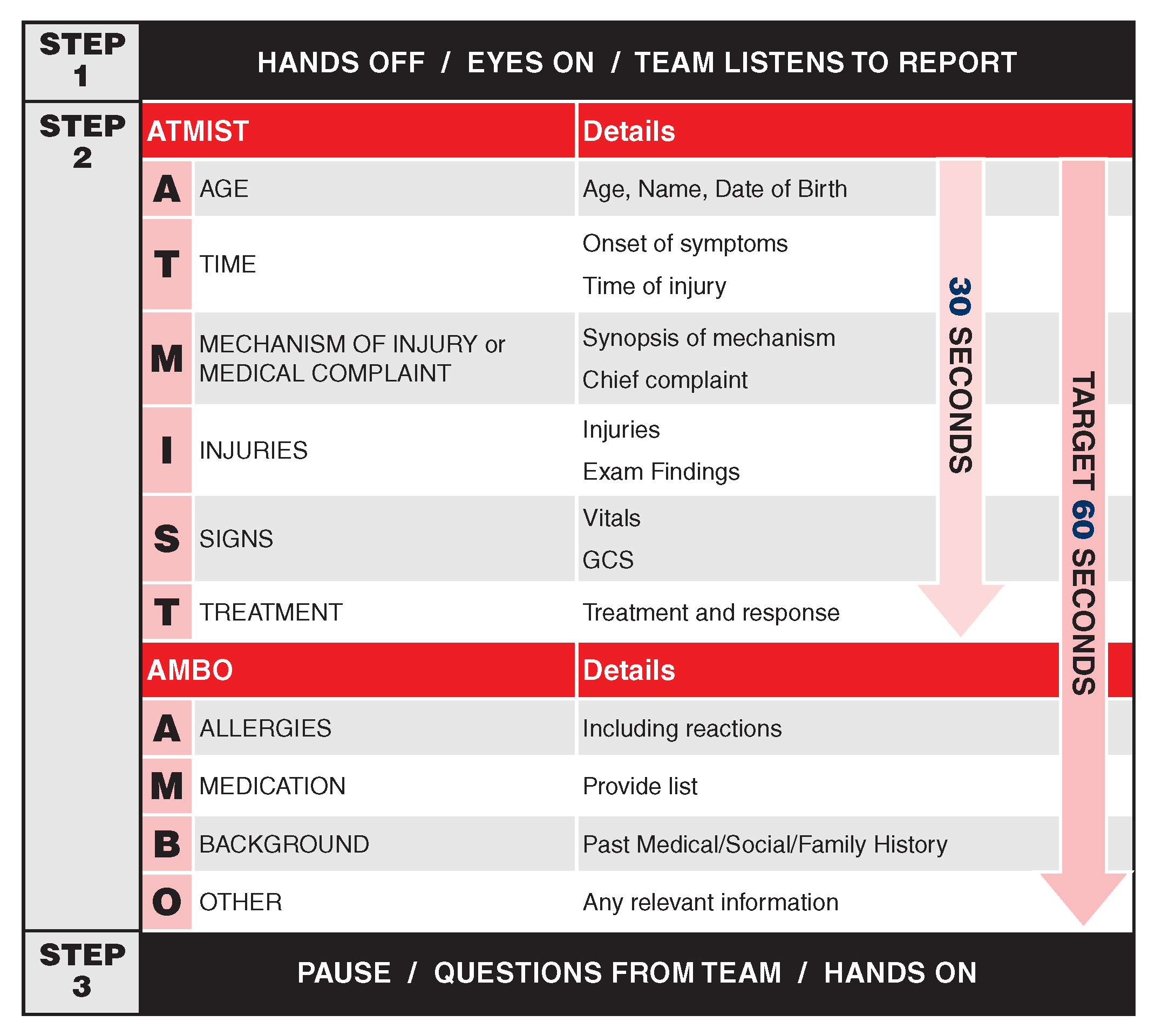 The primary tool used during transitions of care between two providers is ATMIST AMBO. As with all structured tools, ATMIST AMBO is intended to present information in a logical, sequential fashion, with the most critical information presented earlier in the handover report. This tool is used when a paramedic, emergency medical responder, or first responder is transitioning care to another health care provider, including delegations of care in the out-of-hospital environment as well as bedside handovers in hospitals.
The primary tool used during transitions of care between two providers is ATMIST AMBO. As with all structured tools, ATMIST AMBO is intended to present information in a logical, sequential fashion, with the most critical information presented earlier in the handover report. This tool is used when a paramedic, emergency medical responder, or first responder is transitioning care to another health care provider, including delegations of care in the out-of-hospital environment as well as bedside handovers in hospitals.
ATMIST is the recommended tool for pre-arrival notification to hospitals. Pre-arrival notification is required for the following patient types:
- ST elevation myocardial infarction
- Suspected stroke (FAST+ or FAST-VAN+)
- Cardiac arrest (post-arrest or with ongoing CPR)
- Patients meeting major trauma criteria
- Patients who are unstable, as defined by:
- Systolic blood pressure below 90 mmHg
- Heart rate above 130 beats/minute, or below 40 beats/minute
- Respiratory rate above 30 breaths/minute, or below 8 breaths/minute
- Requirement for high-flow supplemental oxygen therapy to maintain oxygen saturation
- GCS less than 13
- Impending airway compromise
- Restraints required
- Active labour and other maternity-related patients
- Patients with spinal motion restrictions in place
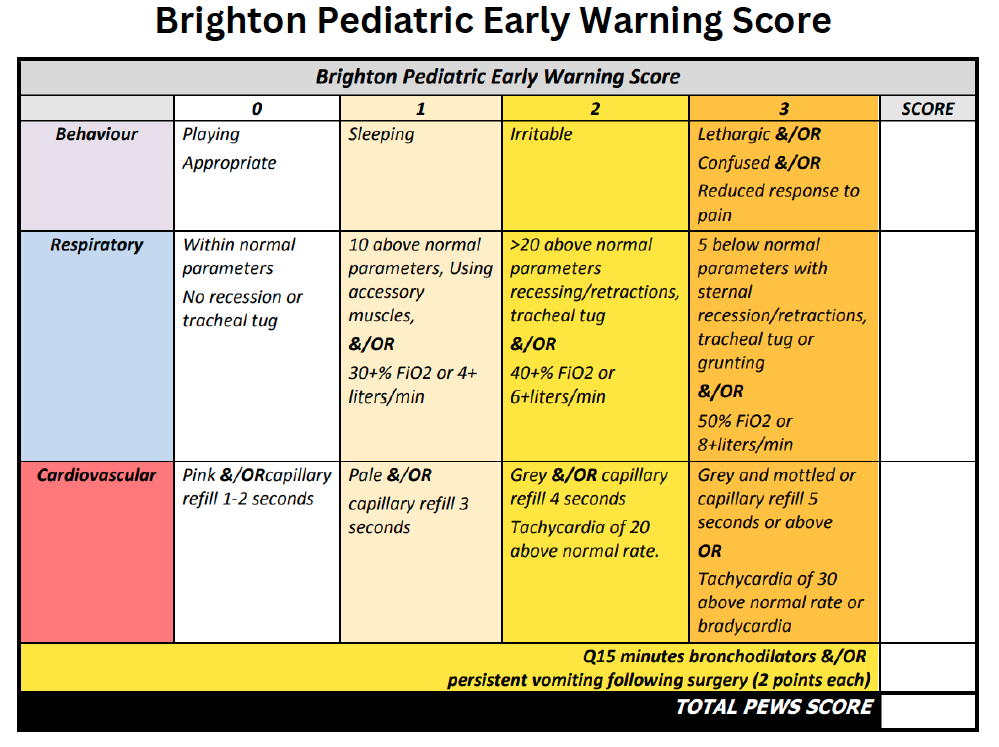
- Pediatric patients with a PEWS score of 5 or higher (or meeting major trauma criteria)
- NB: Pre-arrival notification for pediatric patients is facility-specific. Consult local hospital guidelines.
- Significant drug or other toxic overdose with anticipated rapid decline (e.g., insulin, bupropion, beta blockers, tricyclic antidepressants, etc.)
- Suspected Covid or other infectious disease (e.g., tuberculosis, ebolavirus disease)
- Mass or multiple casualty incidents
- Interfacility transfers arriving from an airport
- Any predicted need for immediate pharmaceutical or therapeutic intervention upon hospital arrival
Paramedics should consider notifying hospitals prior to arrival in cases where:
- Paramedic discretion results in a heightened concern for patient condition
- High profile patients that may require extra security or crowd control
- Ischemic emergencies (e.g., leg or testicle)
- Ocular emergencies with vision loss
- Active atraumatic bleeding (e.g., epistaxis, vaginal or gastrointestinal bleeding)
Triage reporting may follow the ATMIST structure, but workflows vary between health authorities, and providers will need to remain flexible to the requirements of individual facilities and staff.
For the most critically ill patients – particularly during a handover to a team of providers – it is recommended that all providers observe a 20 to 30 second “hands off, eyes on” period where the attending paramedic delivers the ATMIST information without the distraction of on-going care activities and patient and equipment transitions. Depending on patient condition, this may not always be possible, although regardless of circumstances, the lead providers should try to ensure they can speak without interruption or distraction during the handover.
Under ideal circumstances, the complete ATMIST AMBO handover should take no more than 45 to 60 seconds, exclusive of the need for clarifying questions from receiving providers. This time is representative of experienced providers working collaboratively; early use of the tool, by providers unfamiliar with its novelty, may result in longer handovers – this is not considered problematic, and as providers will become more comfortable with the tool, times for handovers will shorten.
Health authority use of ATMIST AMBO varies. Regardless of whether a receiving provider is familiar with ATMIST AMBO, the use of a structured tool helps to organize and simplify a handover report; the onus of ensuring the tool is used rests with the provider delivering the report, not the recipient. Under some circumstances, such as low-acuity patient handovers, there is an opportunity for experienced providers to provide in-the-moment introductions to the tool; BCEHS encourages its paramedics, emergency medical responders, unit chiefs, and clinical operations managers to have those conversations with their colleagues to promote the use of ATMIST AMBO.
ATMIST AMBO should also be used during transitions of care outside of the hospital in alignment with → A13: Patient Care Planning for Handover, and regardless of whether the receiving paramedic or emergency medical responder was intimately involved in the on-scene care of the patient; recall that the purpose of the tool is to ensure critical information is not missed, and that an effective, shared mental model has been created between two providers.
The content of an ATMIST AMBO report can easily be seen on the attached visual aids. When delivering an ATMIST AMBO report, it may help to announce the title of each section before its accompanying information. Templating this material by writing it down prior to handover may help to organize and summarize patient information.
Keep material in each section short, clear, and concise; do not use excessive jargon or technical terminology – different providers use language differently, and concepts and terms may be different in the out-of-hospital and in-hospital realms. Plain language is always better than technical verbiage.
Speak loudly and clearly. Pause where appropriate, allowing time for listeners to hear and understand messages. Conduct handovers such that patient and privacy confidentiality may be preserved whenever possible.
SBAR
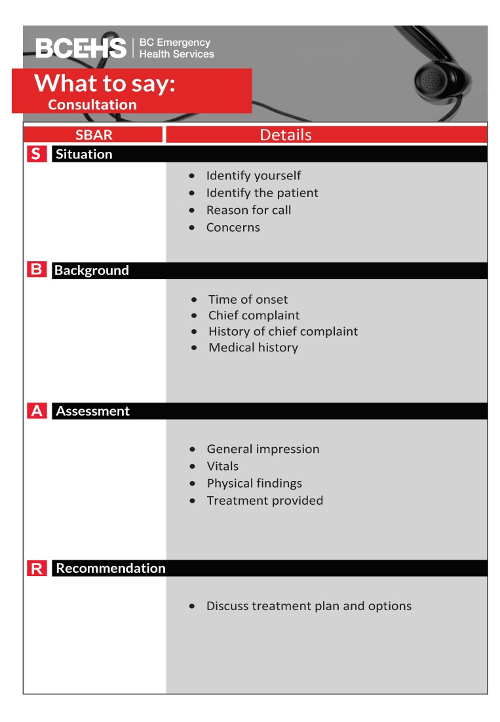 ATMIST AMBO is best suited for the transition of care between providers physically present with the patient. During consultations – such as those with CliniCall – an alternative format is preferred: SBAR. Like other structured communication tools, SBAR presents patient information in a consistent format to enhance shared clinical understanding and is functionally similar to ATMIST AMBO with one key difference –SBAR provides a brief, functional summary of the patient’s status with the goal of making and obtaining recommendations for ongoing care. BCEHS Paramedic Specialists and Emergency Physicians are trained in the use of SBAR and will be familiar with it during all consultations.
ATMIST AMBO is best suited for the transition of care between providers physically present with the patient. During consultations – such as those with CliniCall – an alternative format is preferred: SBAR. Like other structured communication tools, SBAR presents patient information in a consistent format to enhance shared clinical understanding and is functionally similar to ATMIST AMBO with one key difference –SBAR provides a brief, functional summary of the patient’s status with the goal of making and obtaining recommendations for ongoing care. BCEHS Paramedic Specialists and Emergency Physicians are trained in the use of SBAR and will be familiar with it during all consultations.
As with ATMIST AMBO, clarity is preferred over conciseness. Because these are telephone conversations, ensuring that information has been accurately conveyed and understood is important – be sure the connection is clear and that both sender and receiver understand each other, and allow time for recipients to make notes before moving on to another element of the report. It may be helpful to template an SBAR by writing it out prior to making the phone call if time permits.
The use of SBAR for the delivery of patient information in other circumstances is deprecated, and should be replaced by ATMIST AMBO as soon as possible.
Resources
References
- Arora V et al. Patient Handoffs. 2019. [Link]
- Bates DW et al. Research Priority Setting Working Group of the WHO World Alliance for Patient Safety, on behalf of the Research Priority Setting Working Group of the WHO World Alliance for Patient Safety. Global priorities for patient safety research. 2009. [Link]
- Bost N et al. Clinical handover of patients arriving by ambulance to the emergency department - a literature review. 2010. [Link]
- Carter AJE et al. Information loss in emergency medical services handover of trauma patients. 2009. [Link]
- Dawson S et al. Review article: improving the hospital clinical handover between paramedics and emergency department staff in the deteriorating patient. 2013. [Link]
- Evans SM et al. Assessing clinical handover between paramedics and the trauma team. 2010. [Link]
- Evans SM et al. Clinical handover in the trauma setting: A qualitative study of paramedics and trauma team members. 2010. [Link]
- Foster S et al. The effects of patient handoff characteristics on subsequent care: A systematic review and areas for future research. 2012. [Link]
- Goldberg SA et al. Quantitative analysis of the content of ems handoff of critically ill and injured patients to the emergency department. 2017. [Link]
- Iedema R et al. Design and trial of a new ambulance-to-emergency department handover protocol: 'IMIST-AMBO'. 2012. [Link]
- Jensen SM et al. Handover of patients: A topical review of ambulance crew to emergency department handover. 2013. [Link]
- Joint Commission. Sentinel Event Data: Root causes by event type 2004-2014. 2014. [Link]
- Logaraja S et al. An integrated ABCDE approach to managing medical emergencies using CRM principles. 2014. [Link]
- Meisel ZF et al. Optimizing the patient handoff between emergency medical services and the emergency department. 2015. [Link]
- Murray SL et al. Quality of the handover of patient care: A comparison of pre-hospital and emergency department notes. 2010. [Link]
- Owen C et al. Lost in translation: Maximizing handover effectiveness between paramedics and receiving staff in the emergency department. 2009. [Link]
- Sanjuan-Quiles A et al. Handovers of Patients from Prehospital Emergency Services to Emergency Departments. 2018. [Link]
- Shah y et al. Clinical handover between paramedics and emergency department staff: SBAR and IMIST-AMBO acronyms. [Link]
- World Health Organization Collaborating Centre on Patient Safety Solutions. Communication during patient hand-overs: patient safety solutions. 2007. [Link]
- Wood K et al. Clinical handovers between prehospital and hospital staff: Literature review. 2015. [Link]
- Yong G et al. Handover from paramedics: Observations and emergency department clinician perceptions. 2008. [Link]