Confirmation
Download PDF
Open All
E04: Dialysis Emergencies
Updated:
Reviewed:
Introduction
Patients who suffer from an acute or chronic injury or illness to their kidneys are at risk of developing kidney failure. Treatment options depend upon the patient’s clinical condition and comorbidities, ranging from conservative treatment with medication and fluids, to peritoneal dialysis, hemodialysis, or kidney transplantation.
Essentials
- Patients requiring renal dialysis often have numerous other medical problems, including hypertension, diabetes, and cardiovascular disease. Paramedics and EMRs/FRs should be alert to the possibility of concurrent clinical issues.
- Do not attempt to take blood pressures, or initiate intravenous access, in an extremity that has a dialysis shunt or fistula in place.
- Always consider the possibility of hyperkalemia in patients on dialysis or with renal failure.
- Dialysis patients should be conveyed preferentially to a facility capable of providing dialysis services. If the patient is critically ill, convey the patient to the nearest facility. Contact CliniCall for assistance with appropriate clinical pathway.
Additional Treatment Information
Emergency Disconnect Instructions
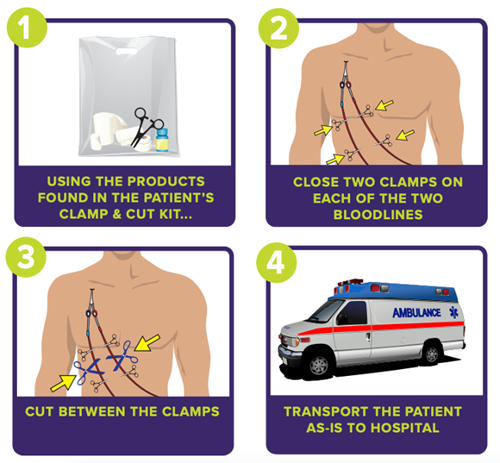
For dialysis patients with a central catheter:
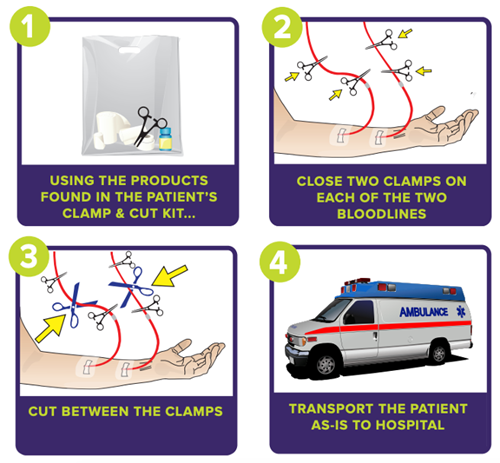
For patients with a fistula or graft:
Referral Information
It may be reasonable to bypass the emergency department in favour of conveyance to the patient’s dialysis clinic. CliniCall consultation recommended to discuss care planning and conveyance options.
General Information
- Peritoneal dialysis uses the peritoneal membrane in the body itself as a filter. This membrane is a fine layer of tissue lining the peritoneal cavity. The peritoneal cavity’s rich vascular supply makes the peritoneal membrane ideal for filtering metabolic wastes and excess fluid from the blood. Dialysis solution is instilled into the abdominal cavity via a surgically inserted Tenckhoff Catheter. Metabolic waste products then pass from the bloodstream, across the peritoneal membranes, and into the dialysis solution. After a period of dwelling time, the solution is drained from the peritoneal space and replaced with a fresh solution.
- In hemodialysis, blood is pumped from the body through special tubing into a dialysis machine via a surgically inserted catheter or arterio-venous (AV) fistula. This typically occurs 3 or 4 days per week at a dialysis centre but can also be performed daily at home. A hemodialysis machine removes waste products and excess fluid from the blood and, as such, acts as a type of artificial kidney. The blood passes through a dialyser (filter), which also assists in balancing fluids and electrolytes in the blood. The machine then returns the filtered and cleansed blood to the body at the same rate at which it was removed.
- Patients undergoing hemodialysis will have a long-term catheter or shunt placed for this procedure. Catheters are typically placed in the upper chest and shunts are typically placed in an arm or forearm. The shunt is created by anastomosing a vein and an artery; turbulence can be felt on the shunt when it is palpated and a bruit can be heard when it is functioning properly.
- Common complications of dialysis treatment include:
- Infection at the shunt or catheter site, or systemically
- Disequilibrium syndrome develops when a shift of metabolic waste and electrolytes occurs, causing weakness, dizziness, nausea and/or vomiting, and seizures
- Hypotension can cause altered LOC, angina, seizures, or arrhythmia, and typically responds to a small fluid bolus of 250 mL normal saline
- Occlusion or disruption of the Tenckhoff catheter
- Some medications are filtered out by the dialyser, limiting their therapeutic effect
- Air embolism
- Shunt bleeding typically following a hemodialysis session, which will occur in 1 to 4 tiny holes made by needles
- To treat, apply direct pressure to control. When the bleeding stops, tape over the gauze but do not remove the gauze to check for control as this will usually cause more bleeding. Circumferential dressings, if used, should not be used as this can occlude the shunt and cause clotting. The tape should, at a maximum, envelope about 180 degrees of the extremity.
Interventions
First Responder (FR) Interventions
- Keep patient at rest
- Control bleeding as required
- Position patient based on comfort and prevent heat loss
Emergency Medical Responder (EMR) & All License Levels Interventions
- Convey in position of comfort
- CliniCall consultation recommended to discuss care planning and conveyance options.
- If at a dialysis facility, engage with staff to provide appropriate care to patient
- CliniCall consultation required prior to initiating treatment or emergency disconnection procedures.
- If patient is attached to a home dialysis machine and is critically ill:
- CliniCall consultation required prior to initiating treatment or emergency disconnection procedures.
Primary Care Paramedic (PCP) Interventions
- Obtain vascular access
- → D03: Vascular Access
- Normal saline if systolic blood pressure is < 90 mmHg or if signs of end-organ hypoperfusion exist
- Correct hypoglycemia
Advanced Care Paramedic (ACP) Interventions
- In patients with significant hemodynamic instability or dysrhythmia and a suspicion of hyperkalemia