Confirmation
M11: Neonatal Cardiovascular
Updated:
Reviewed:
Introduction
Neonatal cardiovascular conditions range from vascular problems to congenital cardiac problems. Neonatal vascular conditions can be separated into the pulmonary vasculature and systemic vasculature; congenital cardiac conditions can be further separated into structural problems (congenital heart disease, or CHD) and intrinsic (arrhythmia).
Paramedics and EMRs/FRs must diligently investigate complaints to isolate and identify the underlying problem, while at the same time providing appropriate supportive care. Differentiation between vascular and cardiac problems begins with the antenatal history.
The time of onset of symptoms varies with the severity of the lesion for cardiac and vascular conditions. Acute, non-cyanosis-producing conditions are usually associated with the complete closure of the ductus arteriosus, which normally occurs around day 2 or 3 of life, followed by a brief symptomatic period. These conditions either result in added strain on the myocardium, signs of congestive heart failure, or signs of inadequate tissue perfusion. Acute cyanotic lesions will usually develop soon after birth and can progressively deteriorate as the ductus arteriosus closes. Arrhythmias can be well tolerated by neonates and take days to months before they are noticed.
Increased pulmonary vascular resistance in the neonatal period is usually a result of an inadequate transition to extra-uterine life. It may begin immediately following birth, to a few hours after birth with varying intensity. Decreased systemic vascular resistance is usually a byproduct of sepsis.
The clinical picture of the cardiac problem varies from progressive deterioration with subtle signs, to the acute conditions with obvious signs. In order to determine the precipitating cause, a multisystem approach involving the respiratory and cardiovascular systems is required.
Essentials
- The cardiovascular system assessment entails assessing the patient’s perfusion, four limb blood pressure, assessing the pulse pressure, heart sounds, signs of hepatomegaly, pre- and post-ductal SpO2 measurements, and radiological testing (U/S and x-ray).
- Pre-ductal SpO2 is performed on the right hand and post-ductal on a lower appendage (right or left foot). A pre-ductal SpO2 < 90%, or a difference > 3%, should prompt more investigations.
Additional Treatment Information
- Cyanotic CHD presents as the classic “blue baby,” that is tachypneic with at times no sign of an increased work of breathing. These patients may have an oxygen challenge to assist in determine a cardiac origin. These conditions can continually deteriorate until either pharmacological or surgical intervention is performed.
- An oxygen challenge consists of either monitoring the SpO2 on the right-hand during room air and then with 100% oxygen administration; a difference of > 10% is usually pulmonary in nature
- Non-cyanotic CHD presentation can vary from the asymptomatic neonate with a pre- and post-ductal SpO2 difference > 3%, to an initially asymptomatic neonate that has an acute deterioration at around 3 days of life that begins with poor perfusion, and leads to cardiogenic shock and respiratory compromise. The asymptomatic neonate requires further investigation by a cardiologist. The symptomatic neonate may require pharmacological treatment to bridge the gap before surgical treatment.
- Pharmacological treatment consists of administering Alprostadil which is a vasodilator (Prostaglandin E1) at an initial dose of 0.02 mcg/kg/hr, followed by gradual tailoring of the dose to 0.005-0.1 mcg/kg/hr (usually requires cardiac echo to tailor); consultation with BCCH PICU and/or BCCH cardiology required to increase dose
- Side effects include: apnea; hypotension; bradycardia; hyperthermia; and cutaneous flushing
- Bradycardia in a neonate is defined as a heart rate < 100. The asymptomatic patient requires monitoring and conveyance to the hospital. The symptomatic patient is defined as having poor perfusion (e.g., hypotension, decreased mentation, signs of shock).
- If HR < 60 bpm with adequate oxygenation and ventilation, start CPR
- Medication: 0.01 mg/kg of epinephrine IV/IO
- 0.02 mg/kg of atropine if increased vagal tone or primary AV block
- Consider transthoracic pacing
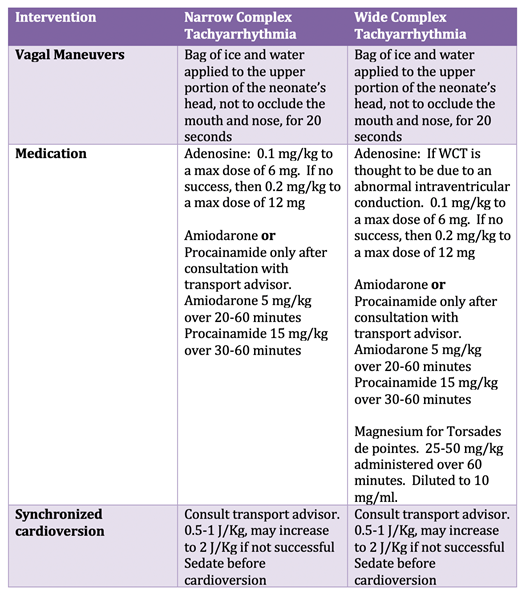
- Tachycardia in a neonate can be classified as either:
- Narrow complex – rate > 220 with a QRS < 0.09 mm
- Wide complex – variable rate (can be normal) with a QRS > 0.09 mm
- In the well perfused neonate with a tachyarrhythmia, paramedics have more time to investigate the cause while preparing a treatment plan. In the poorly perfused neonate (e.g., hypotension, altered mental state, signs of shock), initiate an emergent treatment plan while investigating causative factors.
- Treatment of tachyarrhythmias moves from lowest risk to highest risk to the patient.
- Pharmacological treatment consists of administering Alprostadil which is a vasodilator (Prostaglandin E1) at an initial dose of 0.02 mcg/kg/hr, followed by gradual tailoring of the dose to 0.005-0.1 mcg/kg/hr (usually requires cardiac echo to tailor); consultation with BCCH PICU and/or BCCH cardiology required to increase dose
- Increased pulmonary vascular resistance (PVR) or persistent pulmonary hypertension (PPHN) can result from a difficult transitional period from fetal to neonatal circulation. Oxygen is required to decrease the pulmonary vascular resistance in the first minutes of life allowing the PVR to drop below the systemic vascular resistance (SVR) closing the anatomical shunts of fetal circulation; supplemental oxygen is the first intervention required in these cases. If there is a delay in oxygenation or episode of poor oxygenation in the first hours of life, the PVR can increase, reverting neonatal circulation back to fetal circulation.
- The treatment of PPHN revolves around returning the circulation back to the PVR being lower than the SVR
- Provide supplemental oxygen
- Assess patient fluid status and provide fluid resuscitation if required (10 ml/kg boluses NS to a max of 30 ml/kg)
- iNO – inhaled nitric oxide is a potent pulmonary vasodilator as this can assist in decreasing the PVR; the initial dose is 20 ppm
- Increasing the SVR with inotropes and vasopressors:
- Epinephrine: 0.05 - 1 mcg/kg/min (0.05-0.1 mcg primarily effect B1 and B2 receptors, so increased inotropy/chronotropy and vasodilation; doses > 0.1 mcg also stimulate alpha receptors, resulting in vasoconstriction and increased SVR)
- Dobutamine: 2-20 mcg/kg/min (primarily B1 effects increasing myocardial contractility)
- Norepinephrine: 0.02-0.1 mcg/kg/min (strong alpha effects increasing SVR); normally only used as an addition to another inotrope in neonates
- Vasopressin: 0.1 milliunits/kg/min, increase by 0.1 milliunit every hour to a max of 1.2 milliunits (systemic vasopressor and pulmonary vasodilator at low doses)
- Dopamine: 5-20 mcg/kg/hr (5-10 mcg/kg/hr, primarily B1 effects and > 10 mcg/kg/hr alpha effects)
- While treating the cardiovascular condition, a respiratory distress condition may also be treated as a result of the cardiovascular condition. See Respiratory CPG for respiratory escalation of care.
- Treatable causes of bradycardia:
- Hypoxia
- H+ acidosis – Correct ventilation; in extreme metabolic acidosis, consider sodium bicarbonate (1 mmol/kg)
- Hyperkalemia
- Heart Block
- Toxins – See cardiac arrest CPG
- Trauma – Cushing’s triad of increased ICP; 3% saline at 2.0-5 ml/kg over 10 minutes, or Mannitol at 0.25-1.0 gram/kg over 5 minutes
- Treatable causes of tachycardia
- If potentially a sinus tachycardia (HR < 220, discernable P-waves, rate varies with stimulation, history):
- Fluid bolus for the dehydrated patient (10 ml/kg NS)
- Antipyretic for the febrile patient
- Acetaminophen: 15 mg/kg PO or PR
- Ibuprofen: 10 mg/kg PO
- Analgesia for pain
- Acetaminophen: 15 mg/kg PO or PR
- Morphine: 0.05-0.1 mg/kg IV
- Fentanyl: 1-2 mcg/kg IV/IN/IM
- Ketamine: 0.5 mg/kg IV/IN
- Electrolyte disturbances (due to the variability of disturbance, consult transport advisor for development of electrolyte correction timeframe)
- Hyperkalemia
- Hypocalcemia
- Hypomagnesemia
- Drug Toxicity – unlikely in the neonatal period but should be considered; examples include TCA, cocaine, and methamphetamines
- Risk factors associated with PPHN:
- Hypothermia
- SSRI during pregnancy
- Meconium Aspiration Syndrome
- Congenital pulmonary hypoplasia, congenital diaphragmatic hernia
- Patients with CVS emergencies are at risk of developing coagulopathies from profound metabolic/respiratory acidosis. CBC and Coags should be monitored to direct care with respect to blood product administration.
- Refractory hypotension in the neonate may require a hydrocortisone challenge. Discuss with the transport advisor as to a hypotensive dose (1 mg/kg) or actual cortisol challenge (1-2 mg/kg).
- If potentially a sinus tachycardia (HR < 220, discernable P-waves, rate varies with stimulation, history):
General Information
Amiodarone may cause hypotension if administered too quickly. The risk to the patient must be considered when administering at a quicker rate.
Interventions
First Responder (FR) Interventions
- Maintain thermal stability
- Provide supplemental oxygen as required
- → A07: Oxygen Administration
- Manual airway maneuvers
- Positive pressure ventilation via bag-valve mask
- → B01: Airway Management
- Most pediatric airways can be effectively managed with proper positioning and an OPA/NPA (as per license level) and BVM without any requirements for further airway interventions. The gold standard for airway management is a self-maintained airway. Bag-valve mask is the preferred technique for airway management in pediatric resuscitation and is reasonable compared with advanced airway interventions (endotracheal intubation or supraglottic airway).
Emergency Medical Responder (EMR) & All License Levels Interventions
- Convey to closest facility with notification
- Consider intercept with additional resources
Advanced Care Paramedic (ACP) Interventions
- Consider vascular access and fluid administration if hemodynamically unstable
- Consider intraosseous access
- For bradydysrhythmias, consider:
- EPINEPHrine
- → PR19: Transcutaneous Pacing
- CliniCall consultation required prior to transcutaneous pacing.
- For tachydysrhythmias, consider:
- CliniCall consultation required prior to initiating the below therapies.
- Adenosine
- Amiodarone
- PR20: Synchronized Cardioversion
Critical Care Paramedic (CCP) Interventions
- NIV/Invasive ventilation strategies
- Inotropic and vasopressors for hemodynamic instability
- Vitamins for metabolic derangement
- Electrolyte replacement
- Benzodiazepine infusion
- Antibiotic administration
- Inhaled vasodilator
- Point of care testing
- Blood product administration
- Central Line and Arterial Line monitoring
- Initiation of umbilical lines