Confirmation
PR01: Ambulating Patients
Applicable To
Introduction
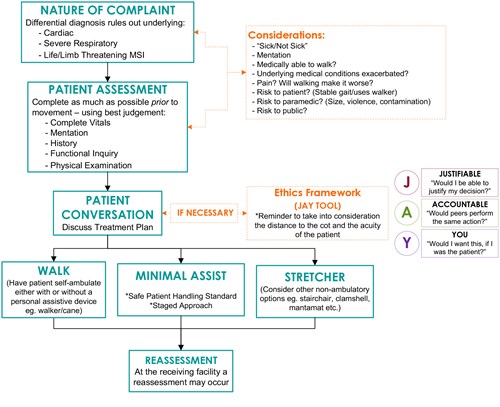
When it is clinically safe for both the patient and the paramedic or EMR, patients should ambulate on their own, or with appropriate support. There are, however, clinical situations in which a stretcher or non-ambulatory method of patient movement should be utilized. Proper assessment will reduce the risk of patient falls and associated risk of injury to patients and paramedics and EMRs/FRs.
The following criteria can be used as a tool to assist in deciding which patients should be conveyed via stretcher, or other non-ambulatory method, and which patients can safely self-ambulate.
Although these guidelines are meant to provide support in the decision about what to do and how to do it, there can be extenuating or unforeseen issues that complicate circumstances. If a situation arises where there is uncertainty about the correct course of action, pause and reflect for a moment. Consider the BCEHS Ethics Framework; specifically, the use of the JAY Decision Making Tool (page 12) for in-the-moment decision-making. The JAY Tool can help individuals to consider all the factors involved before they make a final decision about what to do.
Indications
Contraindications
Procedure
The BCEHS Patient Movement Assessment Tool
Steps for Applying the BCEHS Patient Movement Assessment Tool
The paramedic or EMR may consider some or all of these points when applying the BCEHS Patient Movement Assessment Tool:
STEP 1: Nature of the Complaint/General Impression
- Differential Diagnosis (consider Mechanism of Injury)
- When the differential diagnosis indicates one of the following, these patients warrant a stretcher:
- Cardiac in nature
- Severe respiratory complaint with clinical indicator(s) (e.g., shortness of breath with audible wheezes, decreased SpO2 saturations, etc.)
- Life/Limb threatening MSI
- When the differential diagnosis indicates one of the following, these patients warrant a stretcher:
- Considerations – these considerations may warrant a stretcher or be mitigated by other assistive devices:
- Consider the patient’s acuity:
- “Well" or "Not well”
- Mentation: Is the patient able to follow a conversation? Is the patient cooperative? Is eye movement consistent with intentional cooperation?
- Are they medically able to walk?
- Are there underlying medical conditions that may be exacerbated?
- Is the patient in pain and will walking the patient make the pain worse?
- Consider the risks:
- Risk to the patient; stable gait; do they normally use a walker?
- Risk to the paramedic or EMR/FR; size of the patient; potential for violence or contamination?
- Risk to the public?
STEP 2: Patient Assessment
- Complete as much as possible prior to movement to help confirm or deny your thoughts formulated during Step 1 – using best judgement:
- Complete vital signs (are they normal for THIS patient?)
- Assessment of mentation: GCS and/or LOC x3 (Time, Place, Person) to help determine suitability of ambulation
- History
- Functional inquiry
- Physical examination
STEP 3: Patient Conversation
- A discussion with the patient about the treatment plan allowing them to be part of the decision making process
- Reminder: In this situation the distance to the stretcher is taken into consideration based on the acuity of the patient
Ethics framework (JAY tool)
- Depending on the situation, paramedics and EMRs may need to use this tool
STEP 4: Walk, Minimal Assist, Stretcher
- Walk – self ambulate with or without an aid
- Minimal assist
- PHSA Safe Patient Handling Standard and FAQ
- If it is assumed the patient will need more than minimal assistance, it is recommended the patient be moved using a non-ambulatory method.
- See the Staged Approach to Safe Patient Movement graphic below
- PHSA Safe Patient Handling Standard and FAQ
STEP 5: Reassessment
- At the receiving facility, a reassessment may occur as the patient’s condition and/or abilities may have changed
Notes
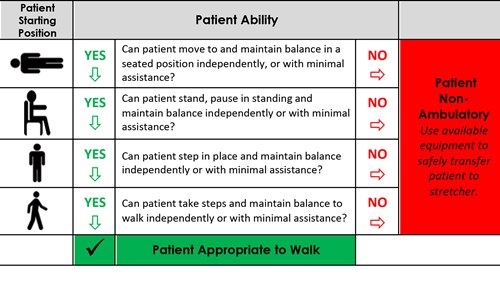
Staged Approach to Safe Patient Movement
- Safe Patient Handling Standard: Please note that this assessment tool works in accordance with the PHSA Safe Patient Handling Standard which states that patients should not be manually lifted if it can be avoided and is not detrimental to the patient’s health. Please review the standard and associated FAQ.
- Manually lifting a patient who can safely walk is not a desirable option. However, a high risk of injury to patient and paramedic or EMR/FR is associated with ambulating a patient at risk of falling. Proper assessment is critical in reducing the risk of falls.
- Do not rely on the patient’s spoken communication to determine if it is safe for them to ambulate. Upon completion of your assessment (as outlined in the Patient Movement Assessment Tool above), proceed to assess the patient’s ability to move. From the patient’s starting position, use the Staged Approach to Safe Patient Movement to guide your decision-making on how to move the patient; this assessment stops when the patient is not able to move on to the next level with no more than minimal assistance. At this point, stop and consider a stretcher or assistive device.
Patient Assessment:
- Before ambulating a patient, be sure the patient:
- Has passed the Patient Movement Assessment Tool (see above) and no contraindications are indicated
- Is cooperative, alert, and able to follow directions
- Can move from lying to sitting and balance while sitting independently or with minimal assistance
- Can stand up and balance independently or with minimal assistance
- Can step in place while maintaining balance independently or with minimal assistance
- Has the ability to self-transfer the distance required (do not over-estimate the patient’s capabilities)
- Important points:
- Clear the environment – ensure no tripping hazards
- Ensure mobility aids, if used, are within reach – on their strong side if possible
- Ensure patient is wearing non-slip footwear if available
- Do not attempt to catch a falling patient; attempt to control the direction of the fall and protect the patient’s head
Procedure for Staged Approach:
Assist the patient from lying to sitting. If the patient cannot do this independently or with minimal assistance, do not walk the patient.
With patient sitting up:
- Check that patient’s feet are flat on the floor and knees and hips are approximately 90 degrees (sitting surface should not be too low), with feet behind knees
- Have patient move to the edge of sitting surface
- Cue patient for proper hand placement (e.g., push on mattress or chair armrests)
Stand to the side of the patient and support the patient at the back (option to hold the patient’s belt if present to stabilize). Use a walker or other mobility device if this is standard practice for the patient.
Assist patient to standing position by reminding patient to have “nose over toes” and to lean into standing (cue patient to push down to get up). The paramedic or EMR should direct the movement and may provide minimal assistance by supporting the patient under their belt, elbow, or wrist. The patient should not grasp the paramedic or EMR/FR and should not be in a position to pull the paramedic or EMR/FR down at the shoulders should they fall.
Ensure patient is able to maintain balance in a standing position. If balance is questionable, sit the patient back down and re-evaluate or proceed with non-ambulatory methods of transfer.
Once the patient is clearly maintaining balance in standing, check that the patient is able to step on the spot while continuing to maintain balance prior to ambulating, using a mobility aid as applicable. If balance is questionable while stepping, sit the patient back down and re-evaluate or proceed with non-ambulatory methods of transfer.
If the patient can step in place and you feel safe to proceed, assist the patient (by guiding and or cuing) to ambulate to the destination. If walking in a hallway, stay close to the wall.
Once the patient has completed their trip, ensure seating surface is positioned squarely behind the patient’s knees, the device is locked as applicable, the device is adjusted to an appropriate height when possible, and then instruct the patient to sit down.
- Provide a verbal reminder to patient: “Can you feel the seat behind your knees?”
- Verbally cue the patient to reach behind to help guide and support themselves while lowering: “Reach behind yourself with one hand to the seat to help let yourself down.”
- Minimally assist the patient as needed to an appropriate sitting or lying position.
Resources
Staged Approach to Safe Patient Movement
Edited May 20/2023 to remove broken links
References
BCEHS. Ethics Framework. 2017. [Link]
Provincial Health Services Agency. Workplace Health - Safe Patient Handling. [Link]