Confirmation
PR05: Patient Decontamination
Applicable To
Introduction
Patient decontamination is any process, method, or action that leads to a reduction, removal, or neutralization of an agent. This can be accomplished by partitioning, binding, or inactivating a contaminant on, or within, a patient. It is intended to prevent or mitigate adverse health effects to a patient as well as aid in protecting emergency first responders, health care facility first receivers, and other patients from secondary contamination. Decontamination also facilitates access to medical care and reduces the potential for secondary contamination of incident response and health care infrastructure.
When required, decontamination is a specific medical countermeasure to toxic or chemical exposures. It should be considered a first aid measure that can be explained to patients as such.
Scene Management
It is critically important to control the environment of a hazardous materials incident. Isolate the scene and deny access to the public, media, and unnecessary responders to prevent needless contamination. Hazardous materials scenes have three concentric control zones:
- The hot zone, or red zone, is an exclusion or restricted area. Chemical protective equipment is required.
- The warm zone, or yellow zone, is an area for decontamination or contamination reduction. Chemical protective equipment is also required here.
- The cold zone, or green zone, is a support zone and is the location in which BCEHS will conduct assessment and treatment. No chemical protective equipment is required in this zone.
All paramedics and EMRs must contact CliniCall to speak with paramedic specialists prior to assessing patients from a hazardous materials incident or chemical exposure. BCEHS does not provide equipment to protect against exposures or to work in hot or warm zones.
It is vitally important that BCEHS paramedics and EMRs work collaboratively with other agencies at the scene to manage hazardous materials incidents and perform appropriate decontamination.
Indications
Contraindications
Procedure
- Evacuate patients to a safe distance prior to decontaminating. Segregate individuals by gender whenever possible.
- Have patients remove all clothing and jewelry prior to performing an emergency (dry) decontamination: this is the most important step and may remove 80-90% of contaminants.
- When conducting a wet decontamination, wash with water and mild soap. Pay close attention to exposed skin folds, axillae, genitals, and feet. Use warm water to reduce the risk of hypothermia and work systematically from head to toe.
- The optimal water rinse time is 15 minutes per person. In cases with large numbers of contaminated patients, a 3 minute water rinse irrigation is permissible to prevent secondary contamination and downstream contamination of health care providers.
- All removed clothing items are considered hazardous and must be properly collected, double bagged, and marked as such for disposal.
- A majority of patients involved in a chemical exposure will not stay at the scene and may find alternative means of transport to hospitals. Surrounding health care facilities should be notified as soon as possible of potentially contaminated patients self-presenting.
 The Three Pillars of the Primary Operational Response (POR)
The Three Pillars of the Primary Operational Response (POR)
Adapted from “Decontamination Guidance for Chemical Incidents,” at 'medicalcountermeasures.gov'
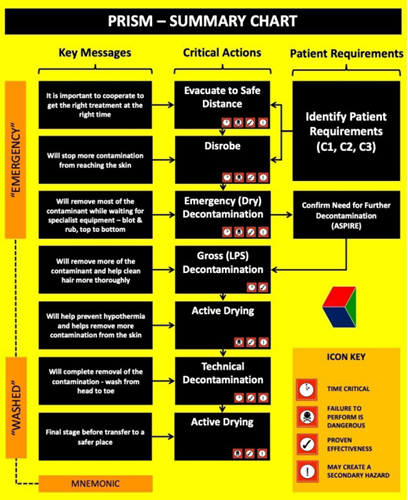
The overriding objectives of the POR are to maximize initial survivability and minimize long term sequelae in individuals who have been accidentally or deliberately exposed to toxic chemicals. The three “pillars” that support these objectives are an understanding of individual needs (patient requirements), an effective communication/management strategy, and clinically effective patient-focused actions.
Patient Requirements
A proportion of patients may be unable to comply with instructions issued by emergency responders. For example, they may be unresponsive, have life-threatening injuries, or may not be able to understand instructions or perform activities without accommodations or assistance. In order to maintain operational effectiveness, all patients need to be rapidly categorized to ensure they are on the appropriate treatment pathway. This guidance document defines three patient categories (C1, C2, C3).
Definition of Patient Categories:
- C1: Patients who are able to understand instructions and perform activities without assistance.
- C2: Patients who are either unable to understand instructions, or who are unable to perform activities without accommodations or assistance.
- C3: Patients who are unresponsive, have life-threatening injuries, or require extensive accommodations or assistance.
Assistance with this form of triage is available from the ASPIRE tool, available from the National Library of Medicine’s CHEMM website.
Communication and Patient Management
Good communication is key to acquiring the trust and cooperation of patients and will maximize the overall efficiency of the initial response phase. Failure to adequately interact with patients may lead to unnecessary anxiety, non-compliance, and security issues at the scene of an incident.
Patient-Focused Action
The goal of the POR is to save lives and improve the clinical outcome of chemically contaminated patients. It is imperative that the following four actions are performed as soon as practically possible:
- Evacuation: Immediate, orderly movement upwind from hazardous areas is a key component of the initial operational response. Inappropriate or delayed evacuation may exacerbate the clinical effects of exposure to hazardous materials and will hamper the effectiveness of subsequent operations.
- Disrobe: The critical, urgent need to safely remove contaminated clothing cannot be overemphasized and is a process that requires effective communication to facilitate patient compliance. The golden rule is that no form of decontamination should be undertaken before disrobing.
- Decontamination: While disrobing will remove the vast majority of a contaminant, exposed areas will require decontamination to remove hazardous material from the hair and skin. There are three forms of decontamination: emergency, gross, and technical.
- Emergency decontamination is the phrase used to emphasize the time-critical process for the immediate removal of hair or skin contamination by any available means and can be divided into “dry” and “wet.”
- Emergency dry decontamination is the default option and should be performed with any available absorbent material.
- Emergency wet decontamination should only be used when the contaminant is caustic (e.g., provokes immediate skin irritation) or is particulate in nature and should be performed using any immediately available source of water at an appropriate temperature (i.e. not exceeding 40º C or 104º F).
- Gross decontamination includes the Ladder Pipe System: two fire engines are parked parallel to form a corridor through which patients pass while being sprayed with a high volume of low-pressure water mist. Alternatively, patients can be sprayed directly with hosepipes using a fogging nozzle.
- Technical decontamination requires the use of specialist decontamination units and associated resources that need to be transported and subsequently deployed at the scene of an incident. In some jurisdictions, technical decontamination is performed at a hospital and so requires conveyance of patients from the scene of the incident. Either way, there will be a delay before technical decontamination can be performed.
- Emergency decontamination is the phrase used to emphasize the time-critical process for the immediate removal of hair or skin contamination by any available means and can be divided into “dry” and “wet.”
Early emergency and gross decontamination compensates for the delayed availability of technical decontamination. It should be noted that the clinical benefits of emergency, gross, and technical decontamination are synergistic: such a “triple protocol” is most effective when performed as one continuous process.
- Active Drying: The act of drying the skin after any form of wet decontamination is a key step. This simple but effective process assists in the removal of contaminants from the hair and skin surfaces, inhibiting further spread of contamination.
Notes
Resources
References
- US Department of Health & Human Services. MedicalCountermeaures.gov. [Link]
- US Department of Health & Human Services. Patient Decontamination in a Mass Chemical Exposure Incident: National Planning Guidance for Communities. 2014. [Link]
- US Department of Health & Human Services. PRISM: Primary Response Incident Scene Management. [Link]