Confirmation
PR44: Pericardiocentesis
Applicable To
Introduction
Emergency pericardiocentesis is needed only for those individuals with hemodynamic collapse secondary to a pericardial tamponade. The lethality of a pericardial effusion has been recognized since the 1600s but the evolution of pericardiocentesis correlates to the advancement of ultrasound techniques. The blind subcostal procedure remains standard when ultrasonography is unavailable, but with a high complication rate. Ultrasound can find a pericardial effusion, but the diagnosis is not radiological; it remains a clinical determination. The hemodynamic consequences of a pericardial effusion are related to the speed and volume of accumulation. Cardiac tamponade represents obstructive shock physiology when the intrapericardial pressure is greater than the intracardiac pressure.
Indications
- Acute cardiac tamponade causing overt hemodynamic compromise; this means peri-arrest or cardiac arrest that requires urgent removal of pericardial fluid.
- Obstructive shock physiology with a radiological identification of an acute pericardial effusion unresponsive to other treatment modalities.
Contraindications
- "Early" cardiac tamponade with minimal or no evidence of hemodynamic compromise may be treated conservatively, with careful hemodynamic monitoring, serial echocardiographic studies (every 2-3 days, or sooner if clinically indicated), avoidance of volume depletion, and therapy aimed at the underlying cause of the pericardial effusion
- Any delay to a centre capable of an emergency thoracotomy
Cautions:
- Severe pulmonary hypertension
- Bleeding diathesis/coagulopathy
- Aortic dissection
- Myocardial rupture
Procedure
Consultation with CliniCall required prior to procedure.
1. Ensure aseptic technique.
2. Select the approach. This is determined by the largest area of pericardial fluid, as noted with ultrasound.
3. Anesthetize the puncture site with lidocaine if applicable and if time permits.
4. Subcostal approach:
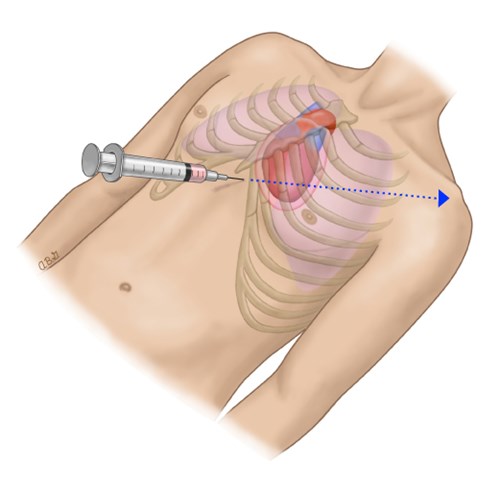
- Carefully consider the location of the mammary artery.
- Introduce the needle substernally 1 cm inferior to the left xiphocostal angle. Once beneath the cartilage cage, lower the needle so it approximates a 30° inclination with the chest wall.
- Aim the needle toward the left mid-clavicle and advance it slowly while continuously aspirating. If no fluid is aspirated, the needle should be withdrawn promptly and redirected. In the absence of ultrasound guidance, withdraw the needle to the skin and redirect it along a deeper, slightly posterior trajectory. The required depth of insertion is affected by the patient's anatomy. In most cases, a 7-9 cm needle is adequate, but longer needles (up to 12 cm) may be needed for obese patients.
- If no fluid is aspirated on the second attempt, withdraw the needle to the skin and redirect it 10° to the patient's right of the last dry needle path. Perform systematic redirected aspirations by working from the patient's left to right until the needle is aimed toward the right neck.
- Once fluid is aspirated stop advancing.
- If ventricular irritability coincides with the advancement of the needle, stop advancing and withdraw slowly.
5. Parasternal approach:
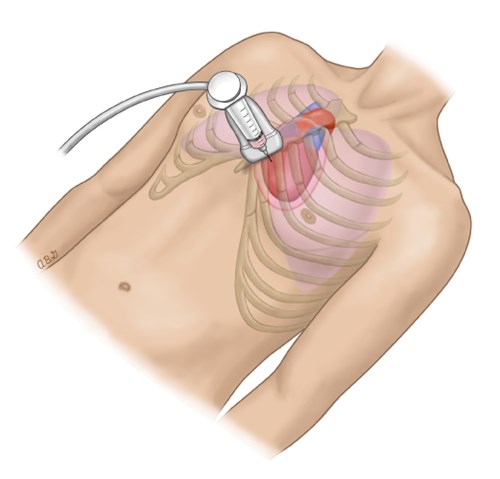
- Insert the needle perpendicular to the skin and over the cephalad border of the fifth or sixth rib immediately adjacent to the sternal margin. The cardiac notch of the left lung exposes the pericardium at this site.
- Avoid puncturing more laterally (> 1 cm) to prevent injury to the internal thoracic (mammary) vessels.
- Once fluid is aspirated, stop advancing.
- If ventricular irritability coincides with the advancement of the needle, stop advancing and withdraw slowly.
- Post procedure, assess for a pneumothorax.
6. Apical approach:
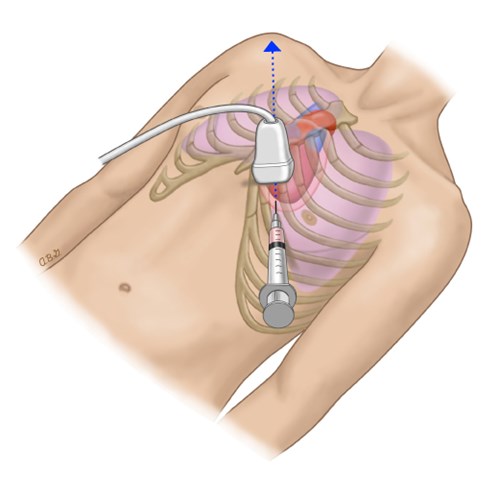
- The apical pericardiocentesis approach reduces the risk of cardiac complications by taking advantage of the proximity to the thick-walled left ventricle and the small apical coronary vessels. However, proximity to the left pleural space increases the risk for pneumothorax.
- The apical insertion site is at least 5 cm lateral to the parasternal approach within the fifth, sixth, or seventh intercostal space. Advance the needle over the cephalad border of the rib and towards the patient's right shoulder.
- Once fluid is aspirated, stop advancing.
- If ventricular irritability coincides with the advancement of the needle, stop advancing and withdraw slowly.
- Post procedure, assess for a pneumothorax.
Notes
- In contrast to the high rates of procedure related complications associated with blind aspiration, multiple observational studies of ultrasound-guided pericardiocentesis report improved safety and success.
- This is a temporizing measure and is not curative. Timely conveyance to a site able to perform a thoracostomy is paramount.