Confirmation
Virtual Palliative Assessments
CPG: Virtual Health
Created: April 16, 2020
Updated: --
Author: Chris Michel
Introduction:
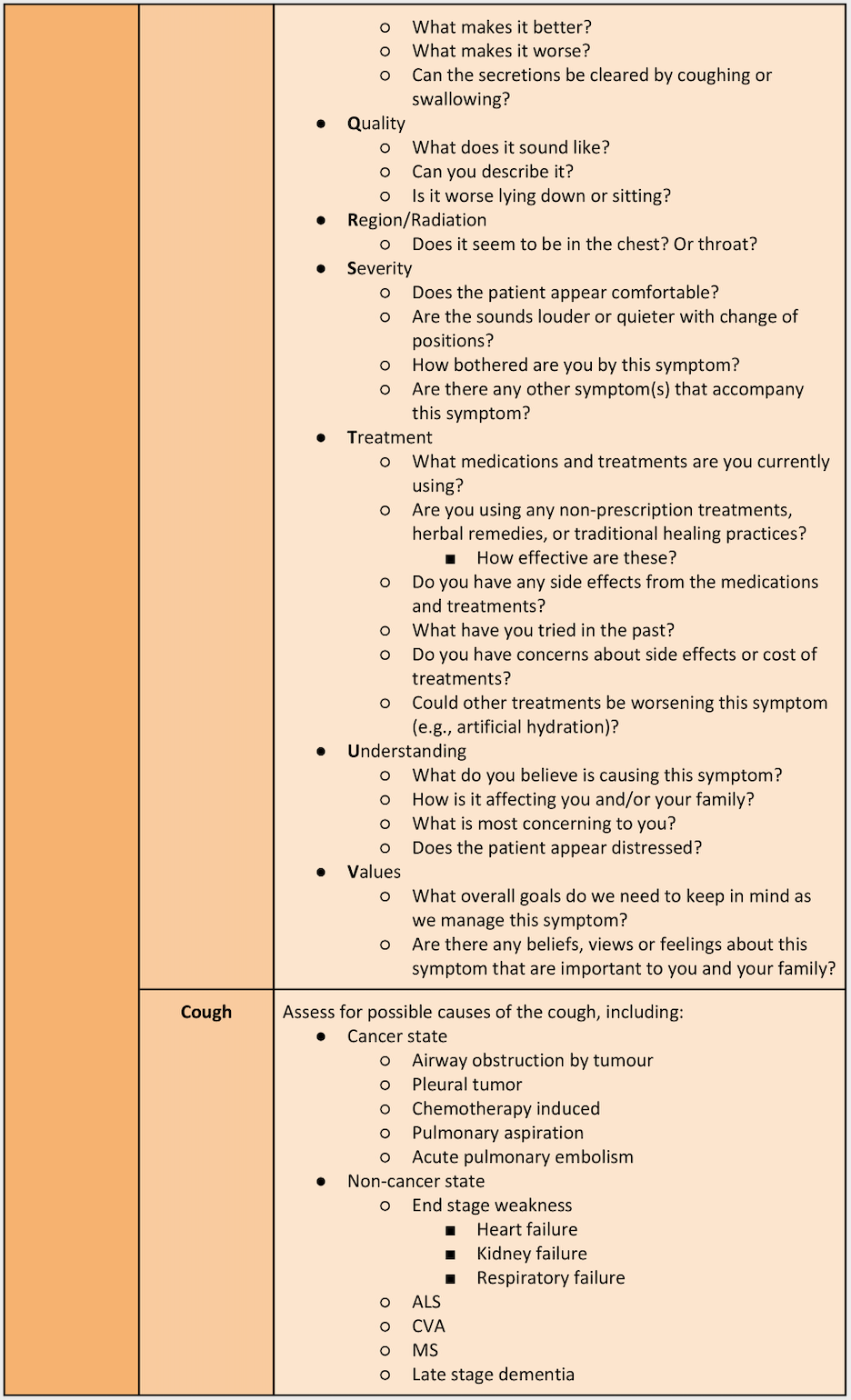
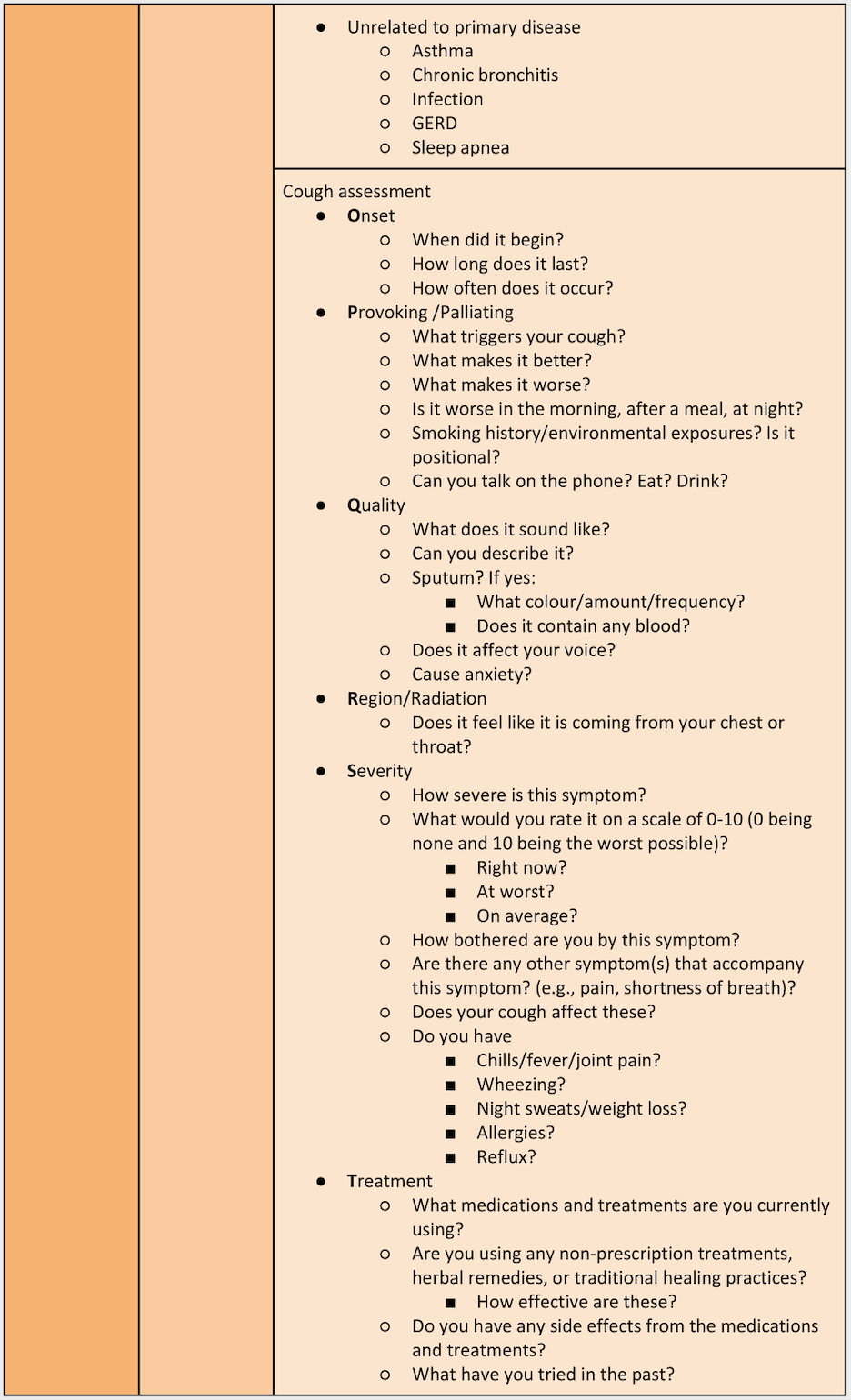
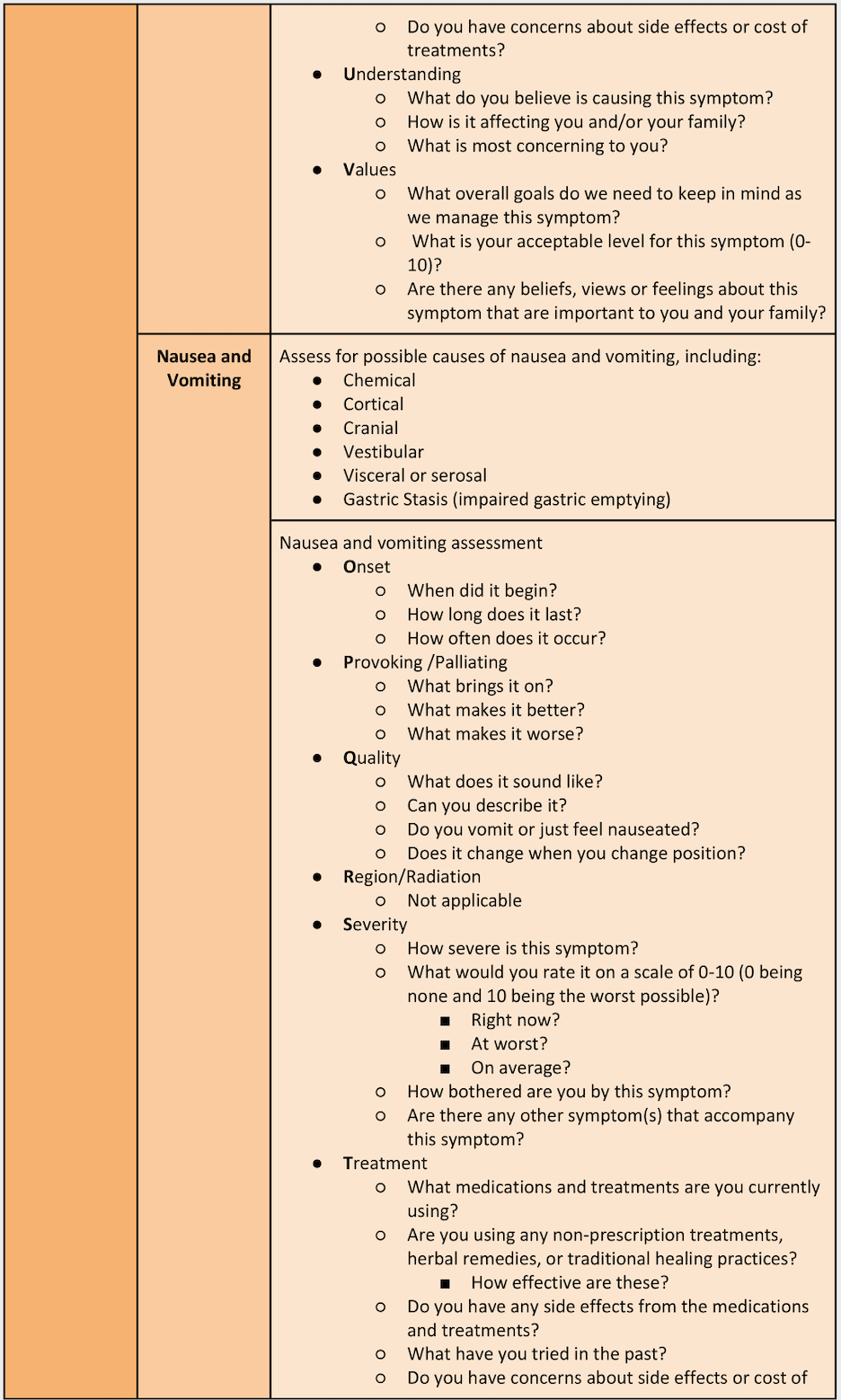
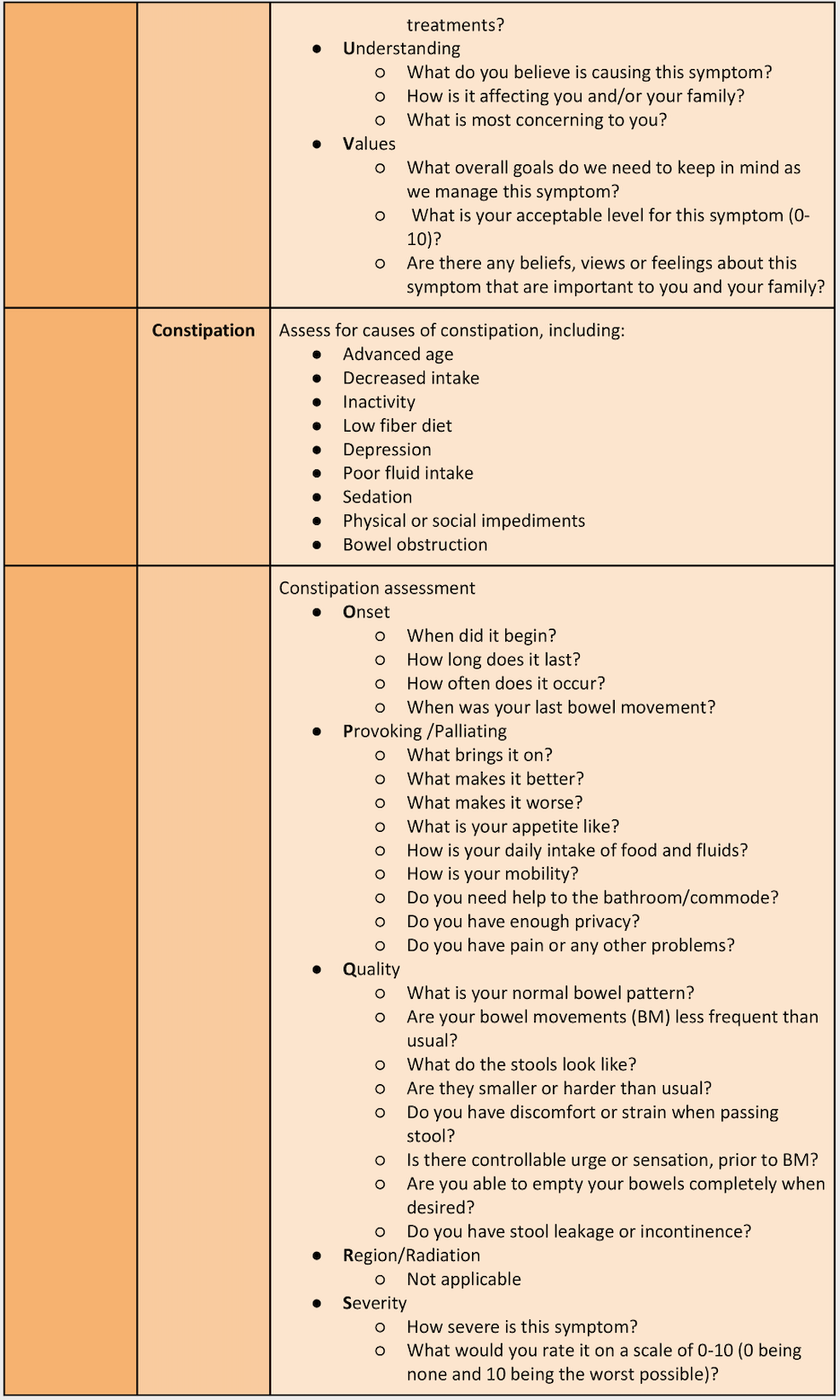
Virtual care is healthcare at a distance and many assessments need to be adapted in the absence of a face-to-face interaction1. Clinical assessments involve the use of tools and instruments which are not available in virtual healthcare settings. Information will need to be gathered in other ways, such as listening to the patient’s cough, or the audible presence of adverse breath sounds, such as wheezing. As with conventional assessments, determine if the patient is experiencing a particular problem and focus on that area first. If no particular problem is present, complete a generalized assessment of the relevant system2.
Paramedics providing palliative care ought to practice “relationship-based care” by adopting a humble, self-reflective clinical practice and positioning themselves as a respectful and curious partner when providing care. In particular, paramedics should seek to respect and learn about Indigenous (First Nations, Métis, and Inuit) and different cultural approaches to palliative care while reflecting on their own values and beliefs. Acknowledging what the differences and the effects of a paramedics’ values and beliefs can have on others is an important step towards cultural humility.
Consult with patients’ usual care team for the creation of a collaborative symptom management plan. If the usual care team is not available or the patient is not under a care team, consider contacting CliniCall (1-833-829-4099 or 604-829-4099) for the creation of a collaborative symptom treatment plan. Where the patient has not followed their symptom management plan, paramedics may encourage the patient/caregiver to administer any medications recommended as part of that plan3,4.
The person is recognized as a palliative patient or at end-of-life by one or more of the following:
-
Person is diagnosed with a life limiting illness
-
Care is currently focused on comfort and symptom management rather than curative interventions
-
Person presents with Goals of Care Designation consistent with treatment in place
-
Person is under care of a physician and/or home care providing palliative care services
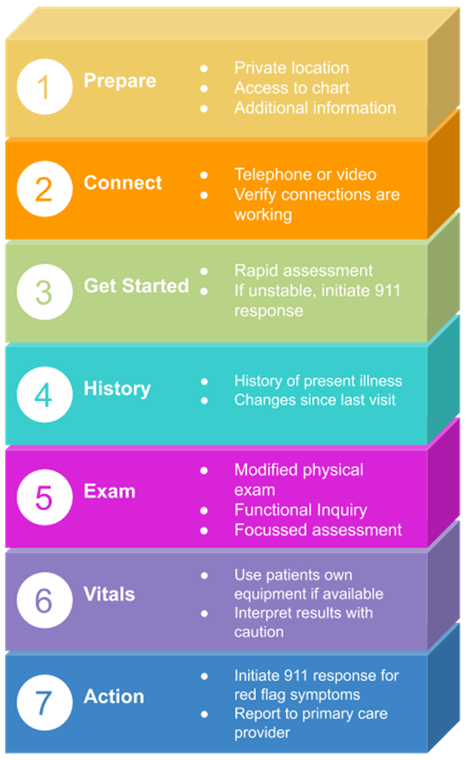
Essentials5:
-
Set-up: Before initiating a virtual visit, make sure you are set up properly, have access to the patient chart, and any additional information that may be required.
-
Connect: Determine the most appropriate method for communicating with the patient (either phone or video chat). Confirm that your audio and video connections are working properly.
-
Get started: Once you begin the visit, perform a rapid assessment to determine if any immediate interventions are needed. For example, does the patient appear very sick, or are they too short of breath to speak? If so, go directly to asking key clinical questions. If no immediate interventions are required, establish what the patient hopes to gain from the visit (i.e., clinical assessment, referral, reassurance).
-
History: Ask questions to determine a history of the present illness.
-
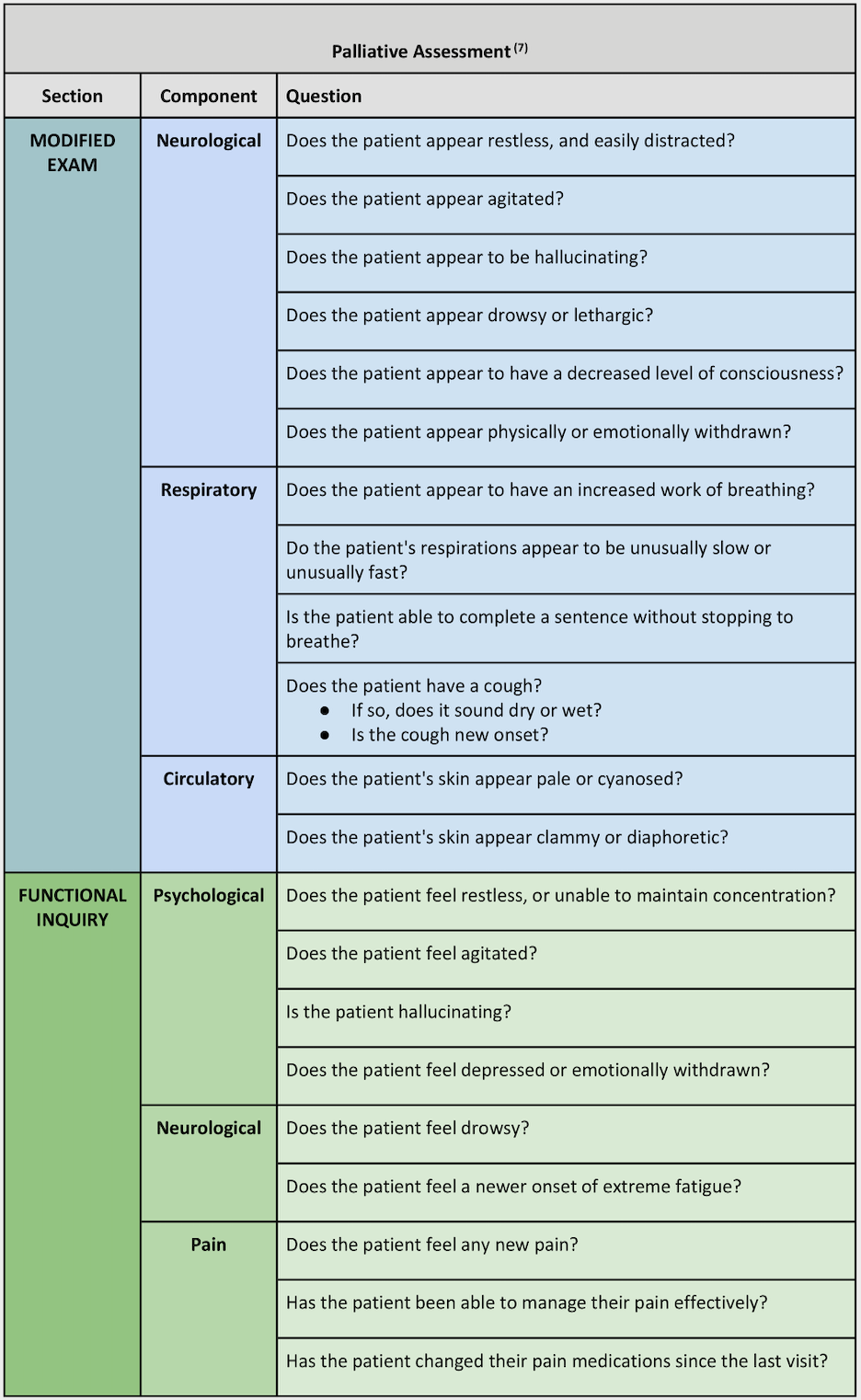
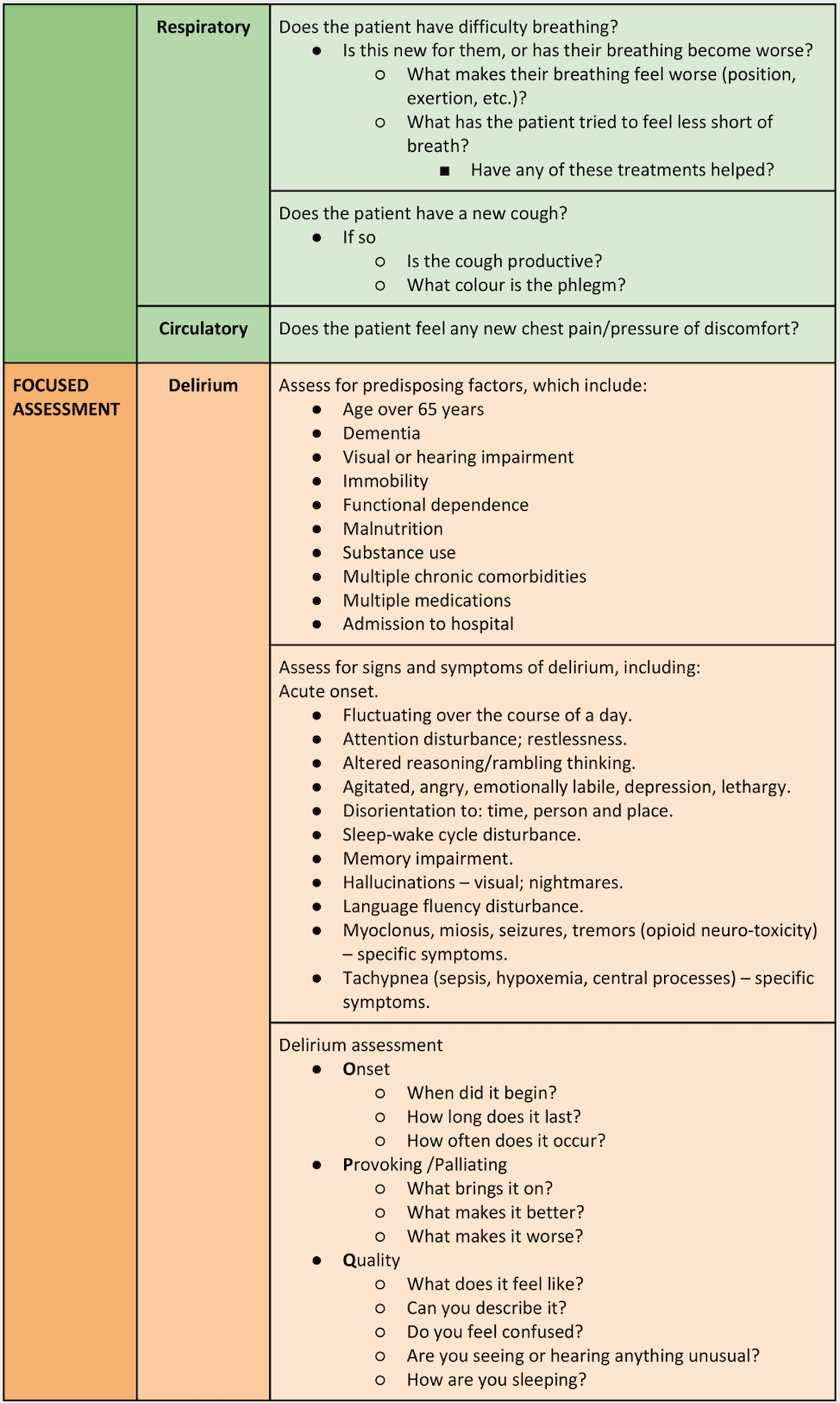
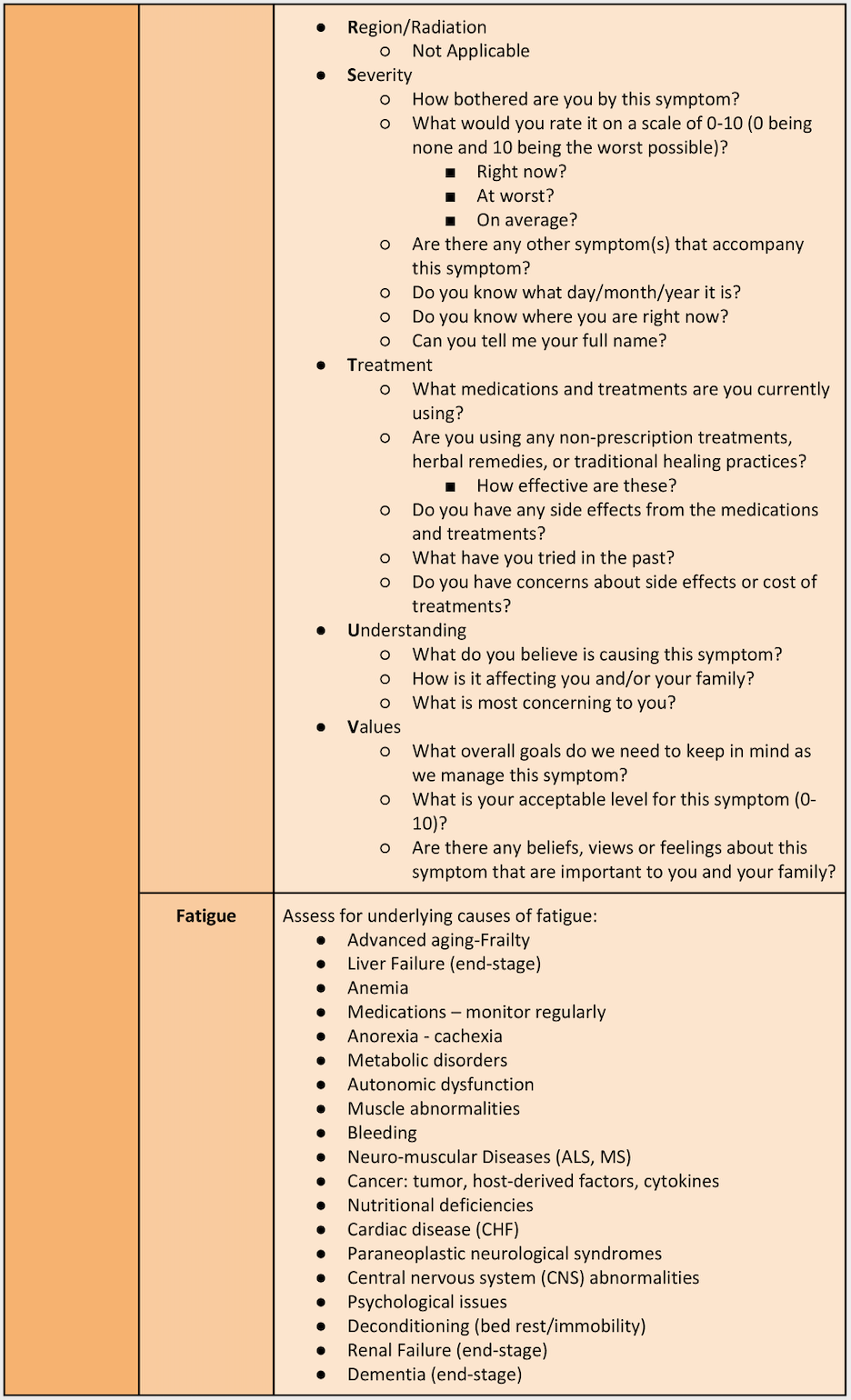
Examination: Perform a modified physical exam and ask functional inquiry questions.
-
Vitals: The patient may be able to take their own measurements if they have access to vitals equipment at home (i.e., blood pressure monitor, pulse oximeter, scale). Interpret results with caution and use them to support findings in the context of your wider assessment.
-
Decision and action: Based on your findings, decide if the patient is able to receive the most appropriate care for their condition and if their symptoms can be successfully managed in their location of choice, or if they exhibit red-flag symptoms and require conveyance to hospital.
-
Report to the patient’s most responsible provider.
Assessment Overview6:
-
The purpose of the Virtual Palliative Assessment CPG is to provide paramedics with guidance in assessing and supporting management of symptoms for people who are currently undergoing palliative care or end-of-life experience. These symptoms are most likely to be nausea/vomiting, pain, delirium/agitation, or dyspnea.
-
Drug and non-drug therapies are equally important.
-
Palliative care is an approach that aims to reduce suffering and improve the quality of life for people who are living with a life-limiting illness.
-
The intent of this care is to provide relief from distressing symptoms, not the treatment of any underlying disease process.
-
Palliative care patients are sometimes conveyed to hospital by ambulance when they would have preferred to remain in their own home. The aim of the palliative care pathway is to ensure that palliative care patients receive the most appropriate care for their condition and remain in their own home as per their wishes, when appropriate.
-
Patients approaching end-of-life may experience pain or other symptoms that cause severe distress. These symptoms are usually managed very well by appropriate interventions and medications administered by the primary care/community health/specialty palliative care team, and sometimes by the family members.
-
Patients who are on the BC Palliative Care Benefits Program have a life expectancy of up to 6 months.
-
Hospice services are available in many communities and can serve to offer additional services to people and their families.
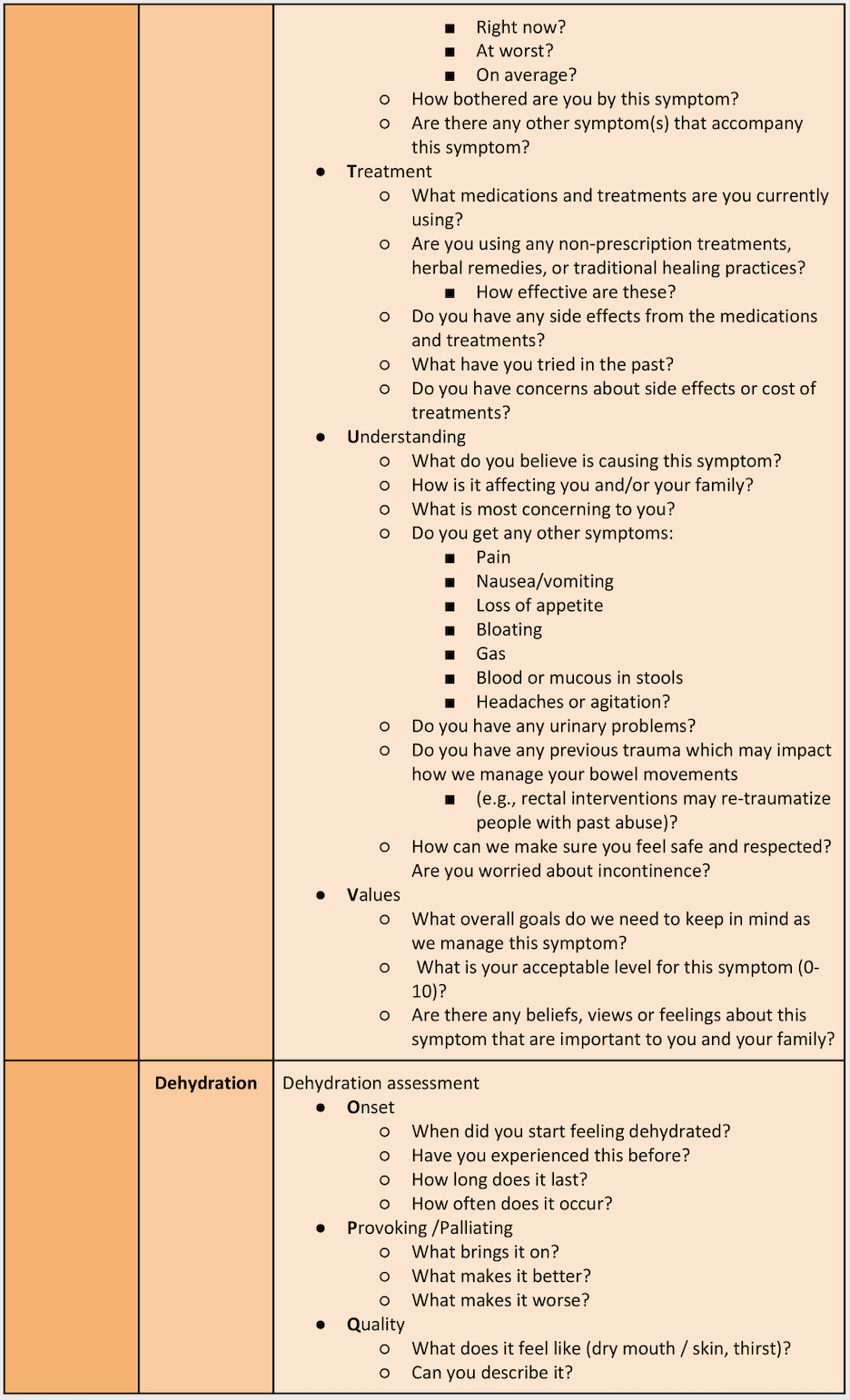
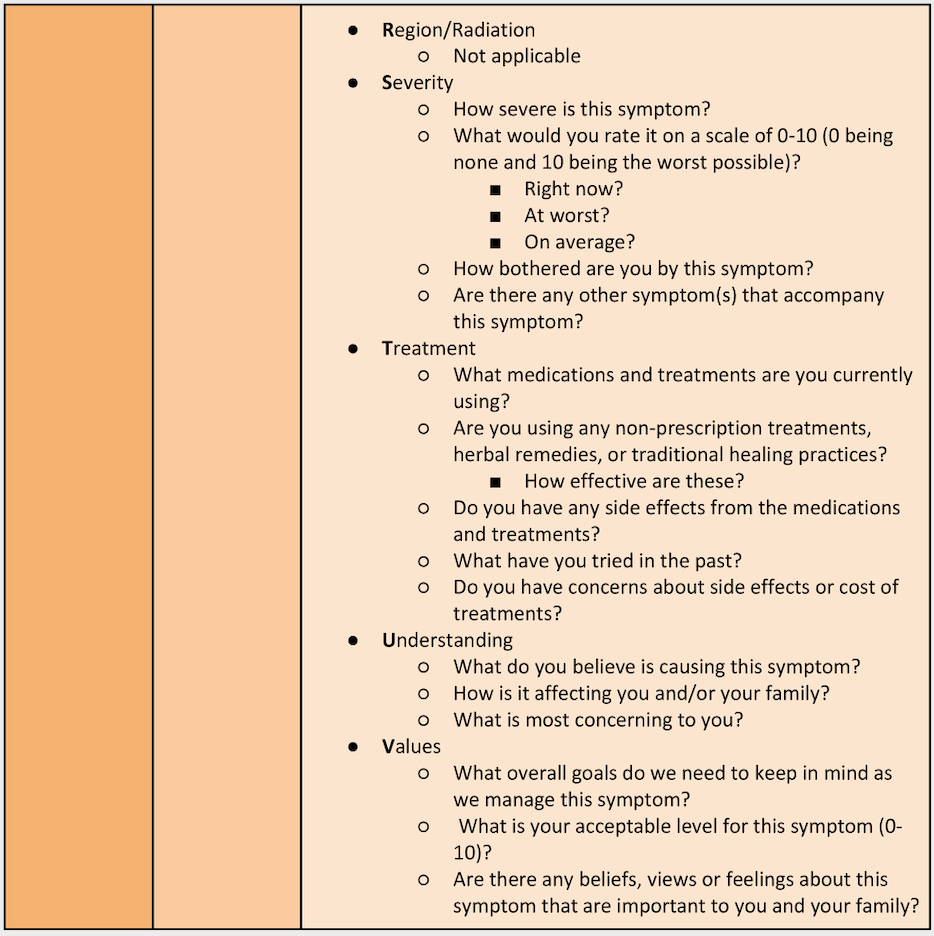
Virtual Assessments:
Risk Identification:
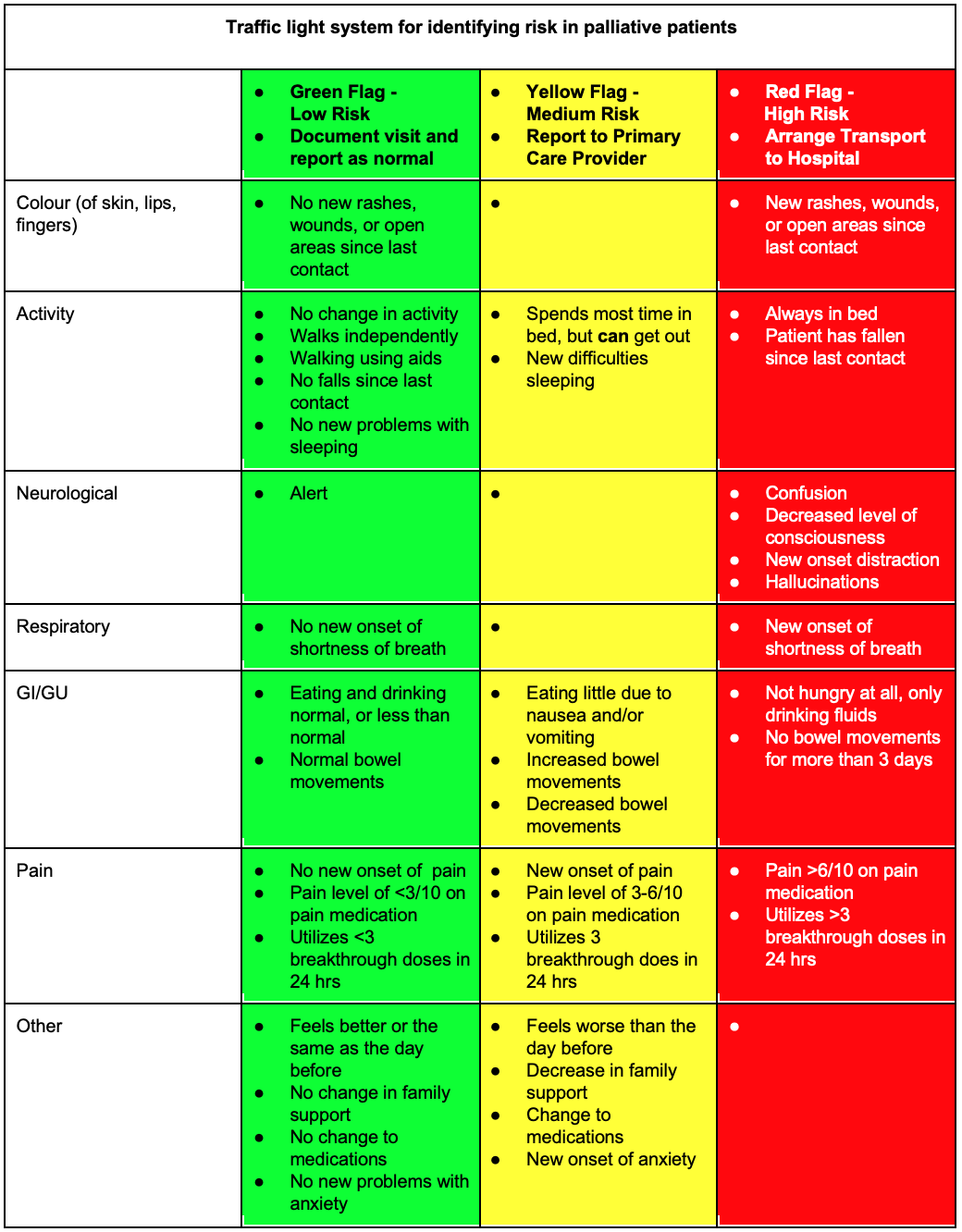
4,7,8
Decision and Action:
- All patients with worsening symptoms (yellow) should be referred to their primary care provider for assessment.
- Patients with red flag symptoms should be managed without delay. Consult with the patients’ usual care team for the creation of a collaborative symptom management plan. If the patients’ usual care team is not available, contact the AHPNS. If neither is available or the patient is not under a care team, contact CliniCall (1-833-829-4099 or 604 829-4099) for the creation of a collaborative symptom treatment plan.
References & Further Reading:
- Telemedicine; Researchers from University of Arizona Detail New Studies and Findings in the Area of Telemedicine (Clinical Examination Component of Telemedicine, Telehealth, mHealth, and Connected Health Medical Practices). Medical Devices & Surgical Technology Week [Internet]. 2018 Jun 10;140. Available from: https://ezw.lib.bcit.ca/login?url=https://search.proquest.com/docview/2047463316?accountid=26389
- Martich D. Telehealth Nursing : Tools and Strategies for Optimal Patient Care [Internet]. New York, NY: Springer Publishing Company; 2017. Available from: http://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,sso&db=nlebk&AN=1442257&custid=s5672081
- iPal [Internet]. Hospice Palliative Care Program, Providence Health Care. 2020 [cited 2020 Apr 16]. Available from: https://ipalapp.com/
- B.C. Inter-Professional Palliative Symptom Management Guidelines [Internet]. BC Centre for Palliative Care; 2019 [cited 2020 Apr 16]. Available from: https://www.bc-cpc.ca/cpc/wp-content/uploads/2019/03/BCPCClinicalBestPracticesInteractiveMarch2019.pdf
- Greenhalgh T, Koh GCH, Car J. Covid-19: a remote assessment in primary care. BMJ [Internet]. 2020 Mar 25;368:m1182. Available from: http://www.bmj.com/content/368/bmj.m1182.abstract
- Palliative & End of Life Care [Internet]. British Columbia Emergency Health Services; 2019 [cited 2020 Apr 16]. Available from: https://handbook.bcehs.ca/treatment-guidelines/adult-guidelines/palliative-end-of-life-care/
- Briggs J. Telephone Triage Protocols for Nursing [Internet]. Vol. 5th ed. Philadelphia: Wolters Kluwer Health; 2015. Available from: http://libproxy.jibc.ca:2048/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=e000xna&AN=1473165&site=ehost-live&scope=site
- HHM Supportive Care Interview. Island Health; 2020.