Confirmation
Virtual Respiratory Assessments
CPG: Virtual Health
Created: April 7, 2020
Updated: --
Author: Chris Michel
Introduction:
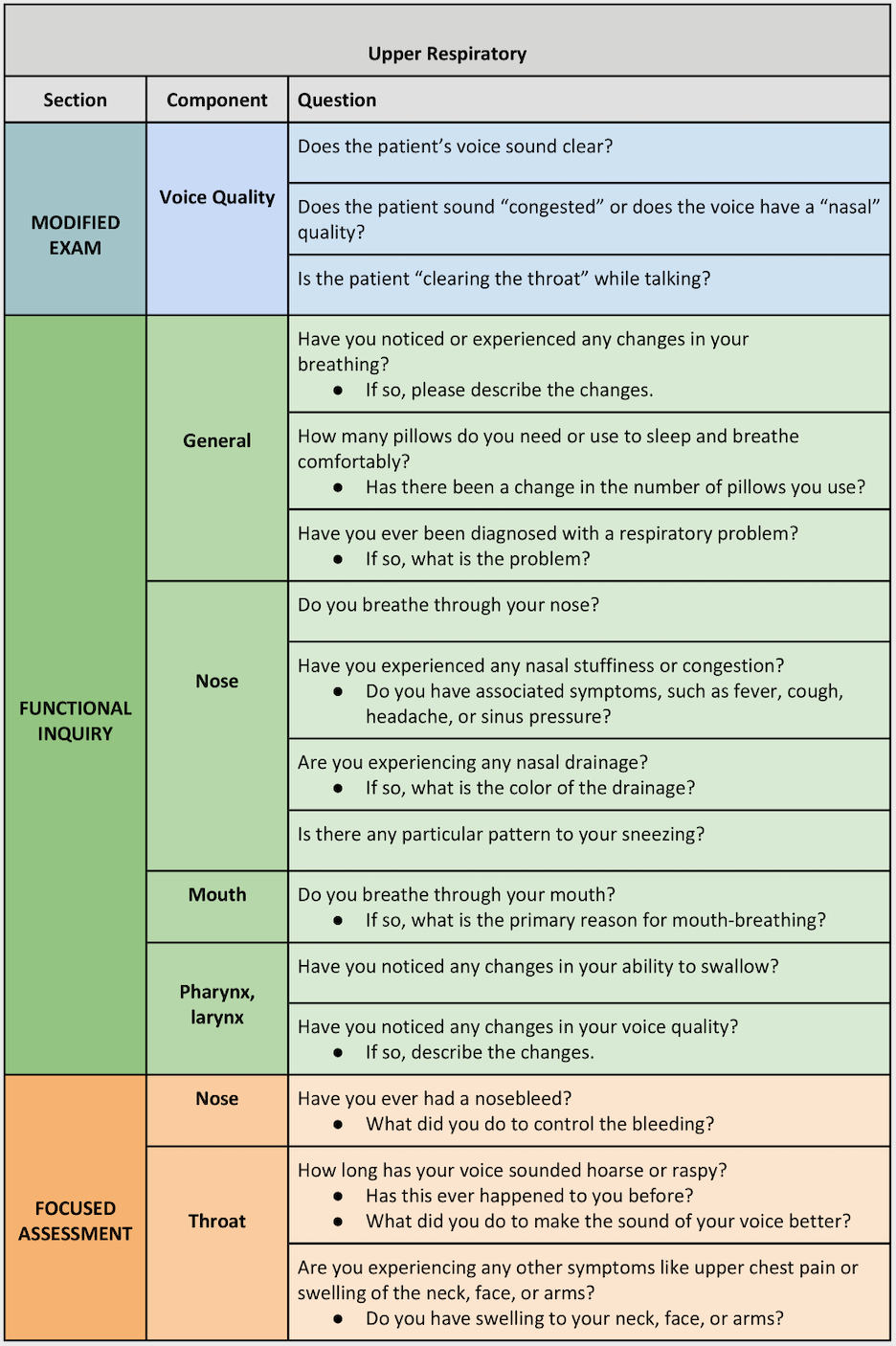
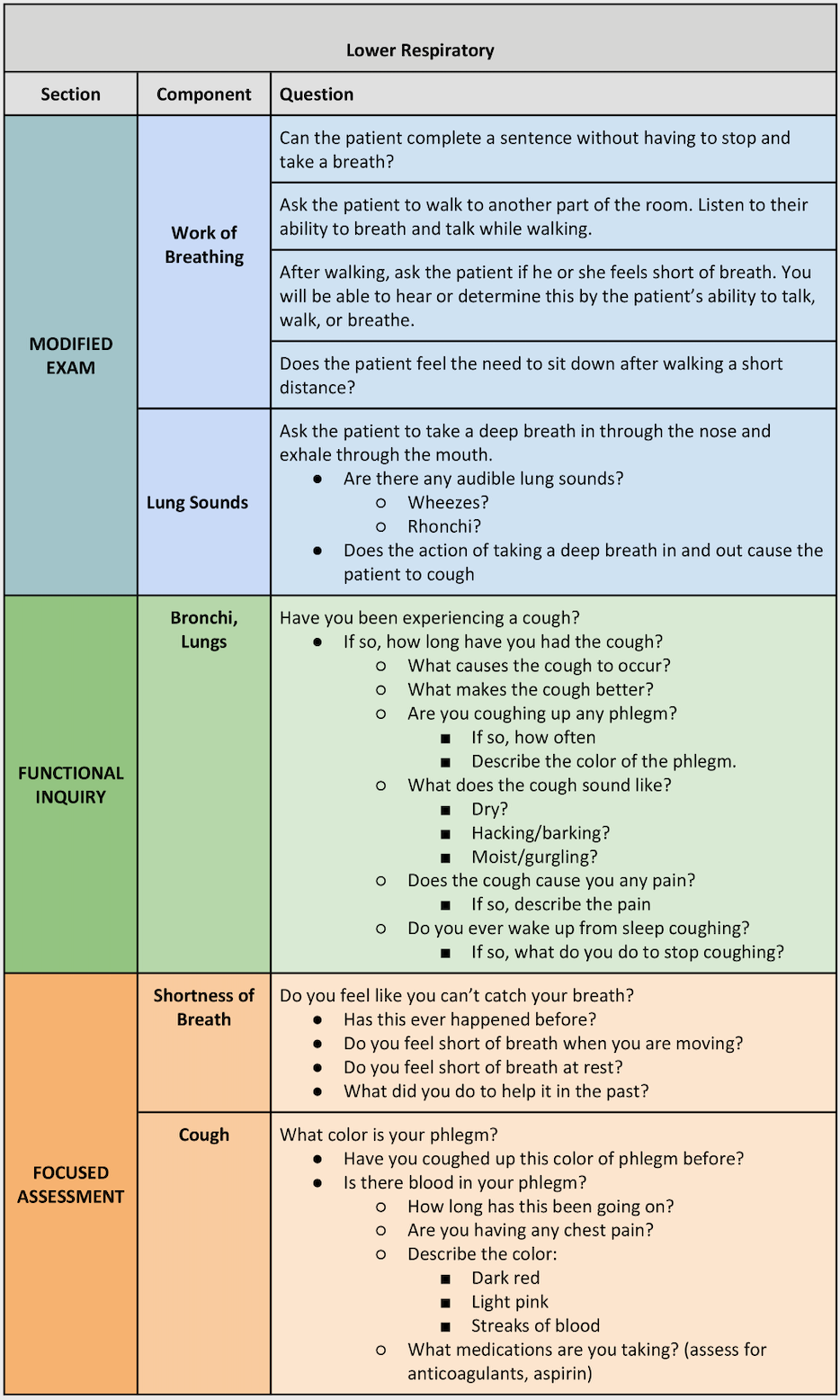
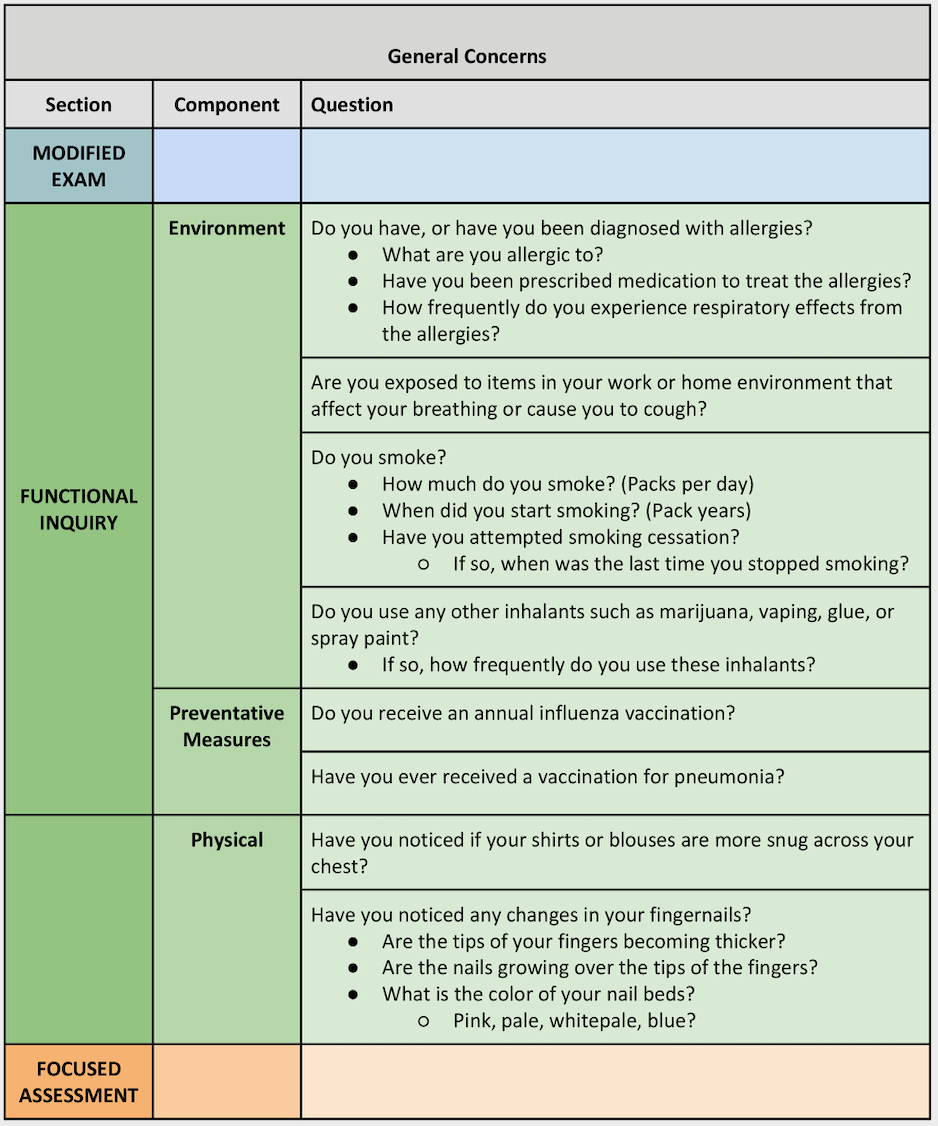
Virtual care is healthcare at a distance and many assessments need to be adapted in the absence of a face-to-face interaction1. General respiratory assessments involve using a stethoscope to listen for lung sounds, which is not available in virtual healthcare settings. Information will need to be gathered in other ways, such as listening to the patient’s cough, or the audible presence of adverse breath sounds, such as wheezing. As with conventional assessments, determine if the patient is experiencing a particular problem and focus on that area first. If no particular problem is present, complete a generalized assessment of the respiratory system2.
Essentials3:
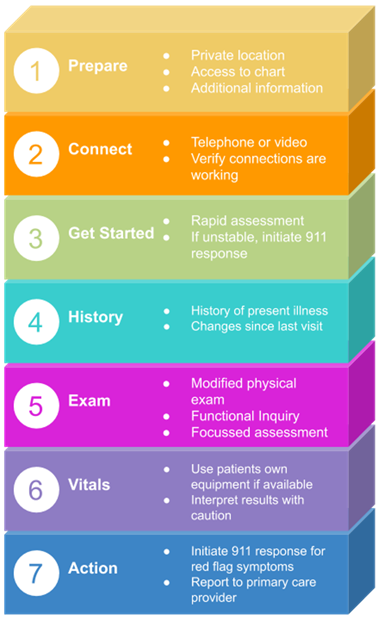
- Set-up: Before initiating a virtual visit, make sure you are set up properly, have access to the patient chart, and any additional information that may be required.
- Connect: Determine the most appropriate method for communicating with the patient (either phone or video chat). Confirm that your audio and video connections are working properly.
- Get started: Once you begin the visit, perform a rapid assessment to determine if any immediate interventions are needed. For example, does the patient appear very sick or are they too short of breath to speak? If so, go directly to asking key clinical questions. If no immediate interventions are required, establish what the patient hopes to gain from the visit (i.e., clinical assessment, referral, reassurance).
- History: Ask questions to determine a history of the present illness.
- Examination: Perform a modified physical exam and ask functional inquiry questions.
- Vitals: The patient may be able to take their own measurements if they have access to vitals equipment at home (i.e., blood pressure monitor, pulse oximeter, scale). Interpret results with caution and use them to support findings in the context of your wider assessment.
- Decision and action: Based on your findings, decide if you should report to the patient's most responsible provider, or if the patient requires immediate conveyance to hospital.
Assessment Overview:
- Because the respiratory system includes two sets of structures, the assessment should be divided into two parts. This assessment can be challenging as it may be difficult to visualize:
- Nasal flaring
- Nasal drainage, colour, and consistency
- Edematous sinus areas
- Chest drainage, colour, and consistency
- Chest diameter
- Nail bed clubbing
- Paramedics traditionally use a stethoscope to listen for lung sounds, but this may not be available when providing virtual care. What will be audible is the presence of a cough and the “noisiness” of breath sounds. The microphone will serve as the “virtual” stethoscope. As with all major body system assessments, determine first if the patient is experiencing any particular respiratory problem. If so, focus on that area first. If not, complete a general assessment of this system2.
Virtual Assessments:
Risk Identification:
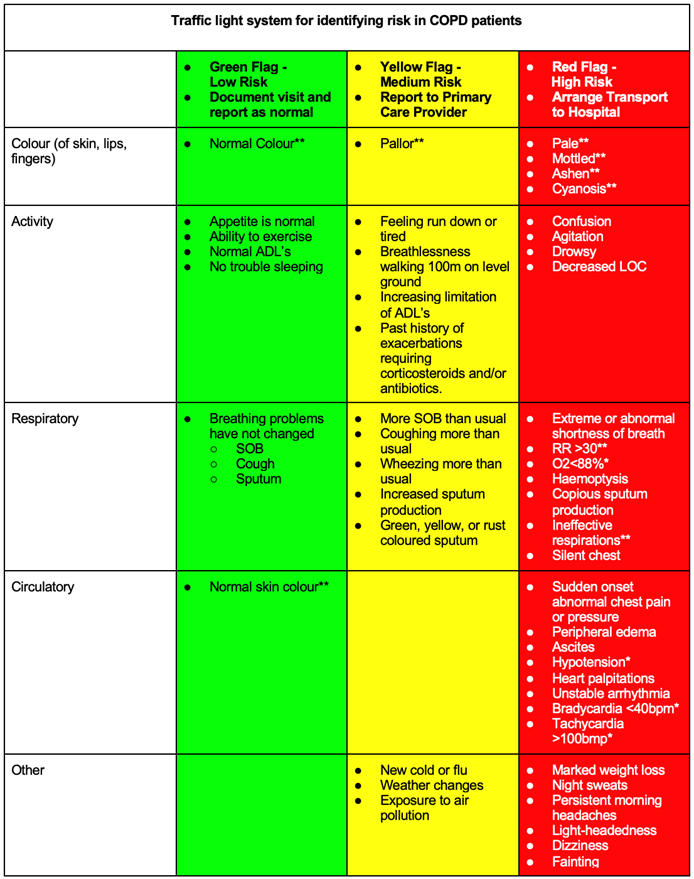
5,6,7,8,9,10,11,12,13
* If able to measure using the patient's supplied equipment
** If able to assess using video conferencing tools
Decision and Action:
- All patients with worsening respiratory symptoms (yellow) should be referred to their primary care provider for assessment.
- If the paramedic does not have an existing history with the patient, they should strongly consider emergency conveyance to hospital for any patients experiencing yellow flag symptoms.
- Patients with red flag symptoms should be conveyed to the emergency department for assessment and treatment. Severe respiratory symptoms include:
- Severe shortness of breath at rest
- Painful respirations
- Chest pain or pressure
- Cold/clammy skin
- New onset of confusion
- Decreased level of consciousness
- Central cyanosis
Additional Treatment Information:
- Many patients living with COPD utilize a COPD flare-up action plan4 which is provided by their primary care provider. Patients should be encouraged to follow their action plan when and if they become symptomatic.
References & Further Reading:
- Telemedicine; Researchers from University of Arizona Detail New Studies and Findings in the Area of Telemedicine (Clinical Examination Component of Telemedicine, Telehealth, mHealth, and Connected Health Medical Practices). Medical Devices & Surgical Technology Week [Internet]. 2018 Jun 10;140. Available from: https://ezw.lib.bcit.ca/login?url=https://search.proquest.com/docview/2047463316?accountid=26389
- Martich D. Telehealth Nursing : Tools and Strategies for Optimal Patient Care [Internet]. New York, NY: Springer Publishing Company; 2017. Available from: http://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,sso&db=nlebk&AN=1442257&custid=s5672081
- Greenhalgh T, Koh GCH, Car J. Covid-19: a remote assessment in primary care. BMJ [Internet]. 2020 Mar 25;368:m1182. Available from: http://www.bmj.com/content/368/bmj.m1182.abstract
- COPD Flare-Up Action Plan [Internet]. British Columbia Ministry of Health, Doctors of BC; [cited 2020 Apr 8]. Available from: https://www2.gov.bc.ca/assets/gov/health/practitioner-pro/bc-guidelines/copd_flare-up_action_plan.pdf
- William McNulty B, Haji G. COPD-Meeting the diagnostic challenge. Br J Fam Med [Internet]. 2014;2:6. Available from: https://www.bjfm.co.uk/media/5866/bjfm_nov-dec_2014_p23-29_copd.pdf
- Chronic Obstructive Pulmonary Disease (COPD): Diagnosis and Management [Internet]. BC Guidelines. 2017 [cited 2020 Apr 9]. Available from: https://www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/bc-guidelines/copd#KeyRecommendations
- Coccia CBI, Palkowski GH, Schweitzer B, Motsohi T, Ntusi N. Dyspnoea: Pathophysiology and a clinical approach. South Afr Med J Vol 106 No 1 2016 [Internet]. 2015; Available from: http://www.samj.org.za/index.php/samj/article/view/10324
- Anonymous. Education: Red flag symptoms - Respiratory tract infections. GP [Internet]. 2014 Sep 15;52. Available from: https://ezw.lib.bcit.ca/login?url=https://search.proquest.com/docview/1564433099?accountid=26389
- IMPRESS breathlessness algorithm [Internet]. The Health Foundation; [cited 2020 Apr 9]. Available from: https://www.networks.nhs.uk/nhs-networks/impress-improving-and-integrating-respiratory/documents/Breathlessness%20algorithm%20IMPRESS%20LSE%20HEalth%20Foundation%20FINAL.pdf/at_download/file
- Lambeth and Southwark Adult Breathlessness Assessment Algorithm [Internet]. NHS Lambeth Clinical Commissioning Group, NHS Southwark Clinical Commissioning Group; 2017 [cited 2020 Feb 9]. Available from: https://www.kch.nhs.uk/Doc/mi%20-%20235.1%20-%20breathlessness%20assessment%20algorithm.pdf
- Non-acute Breathlessness [Internet]. NHS East of England Strategic Clinical Networks; 2014 [cited 2020 Apr 9]. Available from: https://www.respiratoryfutures.org.uk/media/1518/eoe-rscn-breathlessness-algorithm-final.pdf
- Schroeder K, Chan W-S, Fahey T. Recognizing Red Flags in General Practice. InnovAiT [Internet]. 2011 Feb 11 [cited 2020 Apr 9];4(3):171–6. Available from: https://doi.org/10.1093/innovait/inq143
- Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax [Internet]. 1999 Jul;54(7):581. Available from: https://ezw.lib.bcit.ca/login?url=https://search.proquest.com/docview/1781802283?accountid=26389