Confirmation
Clinical Handover & Communicating with CliniCall
First – Is your patient on safe ground: When handing over critically ill patients it is not always obvious if they require immediate intervention or not. For example: you arrive at the hospital ER assisting a patient’s breathing with a BVM, but you are having trouble maintaining SpO2 above 90% and the patient requires suctioning; confidently and politely declare "we are not on safe ground" and declare your emergency. Then give your handover report after the patient is managed and on safe ground. Or you arrive to the ICU with an intubated unconscious patient but does not need immediate intervention, declare “we are on safe ground”. Despite the initial appearance, this puts everyone at ease, and they can focus on your report.
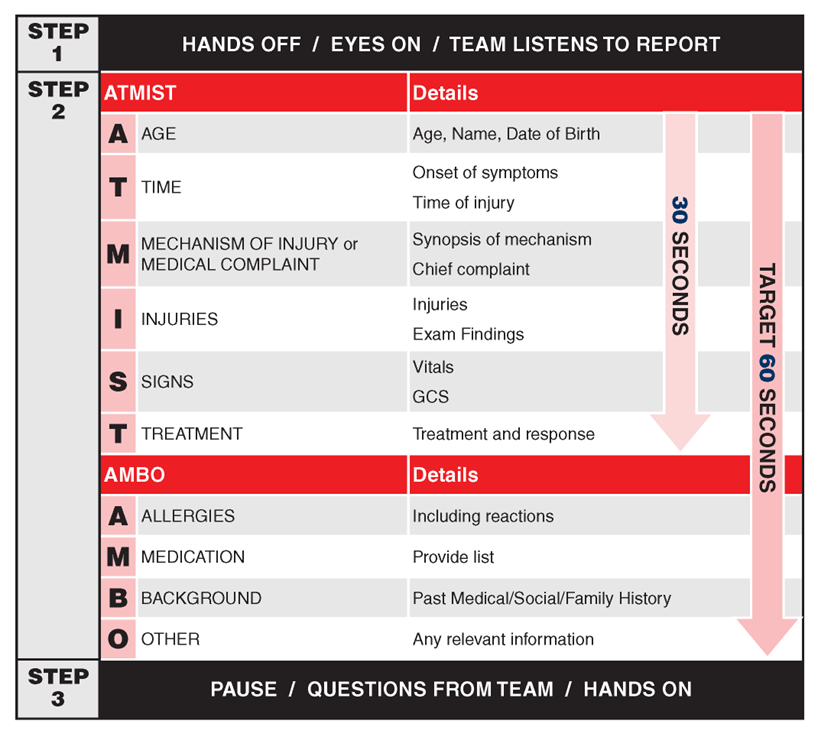
ATMIST AMBO: Used for handover between two care providers and during pre-arrival notification to hospital. See A03: Clinical Handover & Communication for more details.
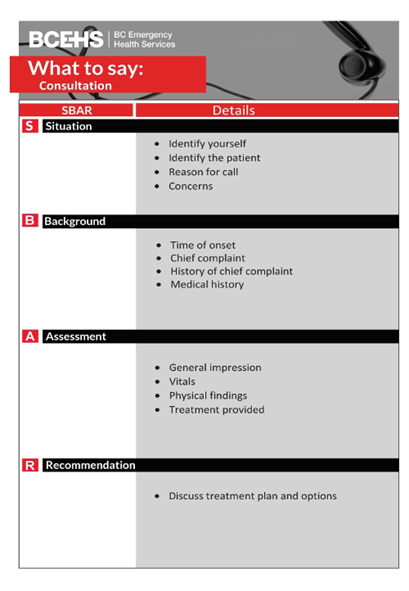
SBAR: Only used when calling CliniCall and speaking to EPOS or a PS for a more concise report, but you can also use ATMIST AMBO if preferred. However, never use the SBAR for anything other than CliniCall consults.
Systems Based Assessment: This is used for more complex patients with multi-system issues. This practice is very common in the hospital environment and the standard reporting structure in the ICU. Critical Care Paramedics and Infant Transport Team Paramedics use this reporting method during interfacility transfers of critically ill patients because these patients often have complex multi-system insults secondary to their illness. Each system is reported regardless of injury, to assess their function. There is a systems-based assessment section in the ePCR which is separate from the narrative section. If you use the systems-based assessment section, the history of chief complaint is still entered in the narrative section. The systems-based assessment and reporting method is rarely used for prehospital calls unless the patient has complex multisystem issues. Please note that this can be a time-consuming report and, in an emergency, ATMIST AMBO may be more appropriate.
|
Problem List |
Primary problem(s) list to manage in order of severity or urgency |
|
Neurological system |
Dependent on injury/illness could include cranial nerve exam, GCS, RASS, FAST VAN, peripheral motor and sensory findings, ASIA impairment score (spinal cord injury), infusion/medications that influence neurological system. |
|
Cardiovascular system |
HR, rhythm/ECG findings, pulses, heart sounds (HS), skin color, cap refill, mottling, ultrasound findings, infusions/medications that influence the heart or cardiovascular system. |
|
Respiratory system |
Resp rate, depth, work of breathing, findings on auscultation/exam (US, CT, CXR), SpO2, blood gases, airway adjuncts (ET tube size/depth) ventilator settings, procedures related to resp |
|
Gastrointestinal & Genitourinary (GI/GU) systems |
GU: urinary catheter, urine output, bladder pressure (if measured). GI: stool frequency, color, consistency. |
|
Skin & Musculoskeletal systems (MSK) |
Skin: color, intact, rashes, lesions, signs of SJS or TENS, burns, lacerations. MSK: broken bones, deformities, splinting and treatments |
|
Hematological & Immune systems |
Any blood work relevant to care, immune system compromise (cancer treatment, biologics) autoimmune disorders |
|
Infectious Disease (I/D) |
Airborne or contact precautions in place and any identified pathogens |
|
Lines & Tubes |
A simplified list of lines and tubes with size and location, e.g: endotracheal tube #4-cuffed, 12cm at gum, CXR 1 cm above carina or IV 24 G, left hand. |
|
Infusions |
List of IV, IO or central line infusions running and include: medication, concentration, rate infused, boluses, location and any complications. |
Required or Recommended Phone call to CliniCall Support Services:
For a complete list of when you should contact CliniCall Support service (to speak to a Paramedic Specialist or Emergency Physician Online Support). Refer to CliniCall Support Services