Confirmation
Vital Signs
Every patient encounter and assessment MUST include at a minimum a baseline set of vital signs. Vital sign frequency is influenced by patient condition, treatments, disposition of conveyance and length of time with patient.
Patient Autonomy: In rare circumstances where a patient refuses to allow vital signs to be taken, you must document the refusal in the narrative section. If refusal of vital signs occurs, explain the risk of refusing and that vital signs are required before we initiate most treatments for the patient’s safety. Ultimately it is the patient’s right to refuse any treatment or assessment offered and we must respect their autonomy to make informed decisions around their body and healthcare. It is never acceptable to perform treatments and/or procedures when a patient who has the capacity to understand risk, refuses to give consent.
Minimum time interval for Vitals: Frequency of vital signs is in context to the patient’s condition, and you may choose to increase the frequency, or in cases where a BP cuff could cause significant pain or patient harm, modify your approach.
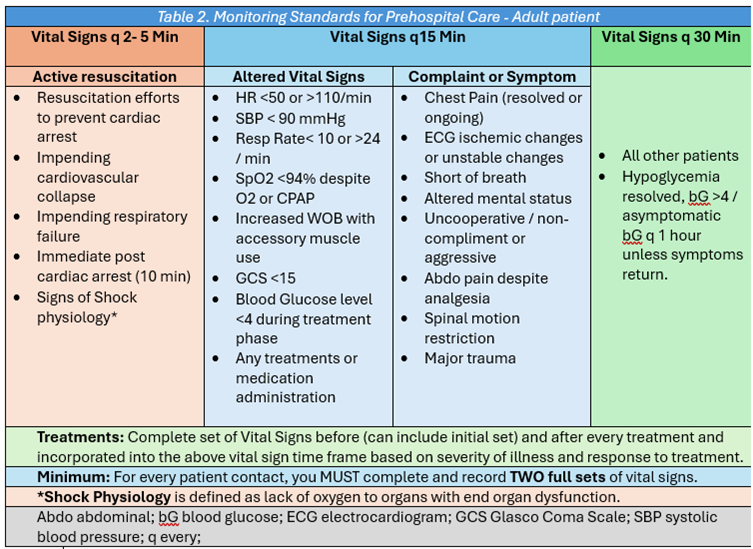
Frequency of vital signs:
- Initial set of vital signs: A full set of vital signs should be completed with initial patient contact.
- Frequency:
- 30-minute intervals: is the minimum interval for patients not requiring treatment and/or no altered vital signs or listed complaints found in Table 2 Monitoring Standard for Prehospital care (below).
- 15-minute intervals: is the minimum interval if the patient has a complaint or symptoms, and/or abnormal vital signs found in Table 2 Monitoring Standard for Prehospital care (below).
- Increased Frequency: dependent on underlying conditions, ongoing treatments, changing or predicted trajectory of trending physiology. Consider increasing vital sign frequency if patient’s condition is anticipated to worsen.
- Shock physiology*: Vital signs can be as often as 2-3 minutes in critically ill patients, especially in the initial resuscitation phase. For example: requiring patient repositioning, fluid bolus and vasopressor administration.
-
*Although patients in shock often present with altered vital sign, shock is not defined by a vital sign. It is defined by lack of perfusion (or oxygen) reaching the tissue of organs resulting in end organ dysfunction. See D01 SHOCK
- Treatments: a complete set of vital signs must occur before and after every treatment regardless of clinical presentation (this can include the initial set of vital signs). Follow up Vital signs then occur based on patient presentation and response to treatment.
- Repatriation transfers: If the patient is being transferred home or to their original care facility and their trending vital signs demonstrate as consistently stable or improvement for a minimum of 12 hours, a longer time interval between vital signs can be considered for these patients for their comfort. A complete set of baseline vital signs are always required before transfer. Follow-up vital signs could occur every hour, if no abnormal vital signs occurred in the past 12 hours, but only if observed and documented by the sending facility.
-
- Air Ambulance environment:
Flying a patient in an air ambulance is a formidable task due to the extreme environmental conditions that challenge both the medical crew and the patient. The aeromedical environment is a blend of relentless noise, reduced oxygen levels, constant motion, and fluctuating temperatures. These elements can amplify stress and strain on the body, making it crucial to adjust medical assessments accordingly. For instance, the noise and vibration can impair the sense of touch and hearing, complicating the process of checking vital signs or listening to heart and lung sounds with a stethoscope. This sounds simple but not anticipating that lung sounds can’t be assessed once in flight have resulted in the death of patients in Canada. However, this challenging scenario is exactly where the skills and adaptability of medical professionals’ shine. It is critical to modify your techniques, often relying on technology and alternative methods to monitor a patient's condition accurately. Understanding and anticipating the effects of G-forces and hypoxia on the body can also guide medical decisions during flights.
“This environment is at best unpredictable, and at worst unforgiving”– Dr. Erik Vu (Executive Medical Director - Air Ambulance & Critical Care Ops, BCEHS)
Pre-plan and modify your approach in the air ambulance setting:
- Vital sign frequency may be increased and the threshold for applying monitoring equipment is lower.
- Anticipate alternative methods for assessing system specific issues in a sensory deprived environment and declare thresholds for intervention before takeoff.
- Crew Resource Management (CRM) strategies between flight crew (pilots and paramedics) should be used before takeoff to discuss the patient’s physiological needs.
- Anticipate physiological changes: Prepare for changes in blood pressure due to unavoidable g-forces, oxygenation due to altitude and increased physiological demands due to stressors (think, O2 supply & Demand).
- Enhance patient comfort: Ensure the patient is warm and secure, minimizing discomfort from vibration and temperature changes, anticipating the potential need for antiemetics, pain control, changes in sedation and vasopressors.
For more information see Dr. Erik Vu’s Interfacility Transport of Acute & Critically Ill Patients in British Columbia
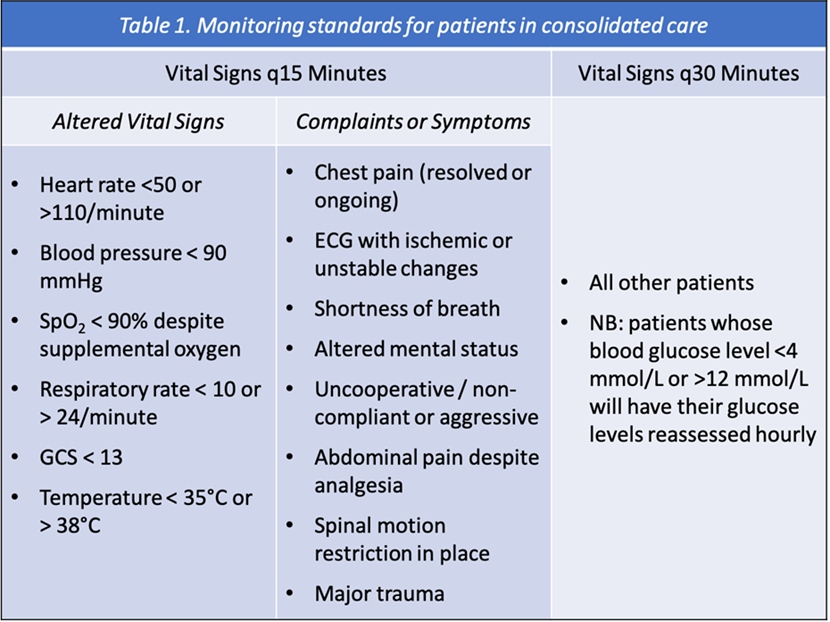
- In-hospital handover delays and consolidation of patient care: The table below can guide you in frequency of vitals to obtain while caring for patient after triage and during a hand-over delay, which also includes consolidation of patients. This chart can also guide you with the frequency of vital signs during transport of patients from a scene or on transfers.
Reference: CPG A04 Duty of Care
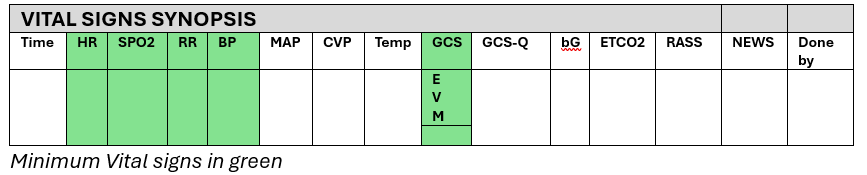
Complete set of Vital signs include: (qualifiers are found under assessment).
- Heart Rate quality and regularity
- Respiratory rate (quality, effort, and any use of accessory muscle
- Pulse Oximetry (oxygen saturation only, heart rate always correlated with pulse).
- Blood pressure (Systolic and Diastolic) *
- Glascow Coma Scale (GCS)
- Skin color and temperature
- Pain Scale – when patient has a pain complaint.
*Blood Pressure can be done either by NIBP or sphygmomanometer and stethoscope and must include both systolic and diastolic pressure. It is only appropriate to do a “BP-by-palp” in extenuating circumstances and MUST be documented in the narrative why this occurred. “BP-by-palp” should never routinely be used and only acceptable due to patient access, or it compromises patient or paramedic safety.
Extended Vital signs and tests when indicated:
- Temperature
- Capillary Refill time
- Pupils – symmetry, shape, react to light, and accommodation
- Blood Glucose
- 4 Lead Electrocardiogram (ECG)
- 12 Lead ECG
- SpCO / SpMet
- EtCO2
- Ultrasound
- Blood Gas and electrolyte analyzer
- Electroencephalogram (EEG)
- Ventilator (equipped with monitoring parameters that must be recorded)
- NEWS2score – Only required by certain ASTaR pathways.
Cardiac monitor should be considered for the following conditions – when available and trained:
- Cardiac Arrest or vital signs absent (VSA)
- Unconscious or altered level of consciousness
- Collapse or Syncope
- Suspected cardiac ischemia
- Moderate to severe shortness of breath
- Cerebral vascular accident (CVA)
- Overdose
- Major or multi-system trauma
- Electrocution (despite appearing fine on initial assessment)
- Submersion injury
- Hypothermia or heat related illness
- Abnormal vital signs
- When requested by staff for transfer
This is the suggested minimum requirement for cardiac monitoring patients and can include any patient you feel would benefit based on clinical presentation. This list does not prevent the transfer of a patient when monitoring is not available. The sending facility, EPOS, CCP-A or Paramedic Specialist, may determine that the benefit of an urgent transfer outweighs the risk of waiting for monitoring to be available. This does not mean ACP must transport based on the above criteria, they must do a risk assessment on the patient before handing off to a PCP or EMR crew.
Modified Blood Pressure or “BP by palp”: Blood pressure with a sphygmomanometer MUST always include both Systolic and Diastolic pressure which requires auscultation. The only instance where a “BP by Palp” is acceptable is in extenuating circumstance where you have limited access to the patient, and/or it is not possible to use a stethoscope. The value of obtaining diastolic blood pressure can’t be overstated, it gives valuable information about perfusion, helps differentiate shock states and guide treatments.
**If you do a “BP by Palp” you must give an explanation in the narrative section with the extenuating circumstances that prevented, you from obtaining appropriate vital signs.
Blood Pressure Post Mastectomy, Lumpectomy or Axillary node dissection: Always respect your patient’s autonomy and their chartered right to refuse any treatment or assessment. Patients who have a mastectomy, lumpectomy (lymph node removal or damage) or auxiliary node dissection may be told to avoid blood pressure monitoring, blood sampling and injections to the arm of the side where those procedures were done to avoid unwanted swelling or lymphedema. Modify your approach to this patient population when possible and do a BP, or injections on the other arm. If the patient had a bilateral mastectomy or lumpectomy, a BP can be done on the patient’s thigh if practical (if you have a BP cough large enough). However, if the patient has healed from the procedure, there is currently no evidence to support the avoidance of a BP to the arm on the same side where a mastectomy, lumpectomy or axillary node dissection occurred (Bryant., 2016). If it is necessary to perform a BP or injection on this arm, explain to the patient the risk vs benefit and only perform the procedure if consent is granted (informed consent). https://pmc.ncbi.nlm.nih.gov/articles/PMC5260339/
Spo2 monitoring, limitations: Spo2 monitoring is almost ubiquitous in prehospital care around the world, but it is critical we know its limitations. When using pulse oximetry, it is important to correlate this with patient presentation and oximetry waveform. When waveform monitoring is available, seeing a consistent wave with dicrotic notch is indicative of a reliable reading. If using a device with no waveform, they are equipped with lights that indicate if it is detecting enough perfusion to calculate an accurate SpO2. When the green light is blinking consistently it will display an SpO2 that can be relied on. It should also be noted that all SpO2 devices will display a falsely reassuring SpO2 in CO poisoning and Methemoglobinemia’s, sickle cell disease, venous congestion and severe anemia.
Spo2 Waveform: Only the waveform with the normal signal (A) below is reliable for obtaining oxygen saturation.
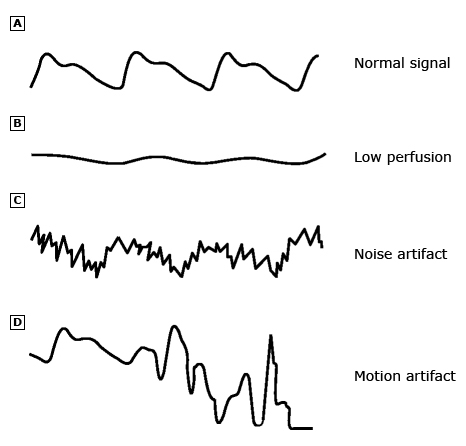
Common pulsatile signals on a pulse oximeter.
- Normal signal showing the sharp waveform with a clear dicrotic notch.
- Pulsatile signal during low perfusion showing a typical sine wave.
- Pulsatile signal with superimposed noise artifact giving a jagged appearance.
- Pulsatile signal during motion artifact showing an erratic waveform.
SPO2 False high readings:
- Skin pigmentation: Paramedics should be aware that current SpO2 monitors have a racial bias for SpO2 monitors to falsely report higher saturation in non-white patients then the actual oxygen saturation. With the current frequency of light and software used in SpO2 monitors melanin interferes with the reading and results in a margin of error as high as 6 %. During the COVID-19 pandemic, black people were found to have been under triaged and under treated due to false high readings which delayed treatments. This also erodes trust in the health care system as many of these patients were already marginalized people. This affects all non-white people with varying degrees based on the amount of melanin present in their skin. This should be kept in mind when treating non-white patients when they have a complaint of SOB and a relatively normal SpO2, they may actually be hypoxemic.
- Carbon monoxide (CO): carboxyhemoglobin is interpreted hemoglobin fully saturated with O2 by SpO2 monitors (not equipped with co-oximetry), this results in a false high reading. If you ever suspect CO poisoning the pulse oximeter is NOT to be relied on. For context, if 70% of hemoglobin is bound with carbon monoxide, Standard pulse oximeters will display 90% SpO2 while the true SpO2 is 30%. The only time SpO2 should be used in suspected CO poisoning is when you have a Co-Oximeter or Rainbow probe (Masimo on certain LP15 monitors) and obtain the SpCo level.
Abnormal Vital Signs
- Adult: Please refer to the NEWS2 score for abnormal adult vital signs in CPG A02: Patient Assessment Also consider using CPG A04 Duty of Care
- Pediatrics: Pediatric Assessment Triangle (PAT): For pediatric patients use the PAT for your initial assessment to look for immediate signs of shock or predicted decompensation.
-
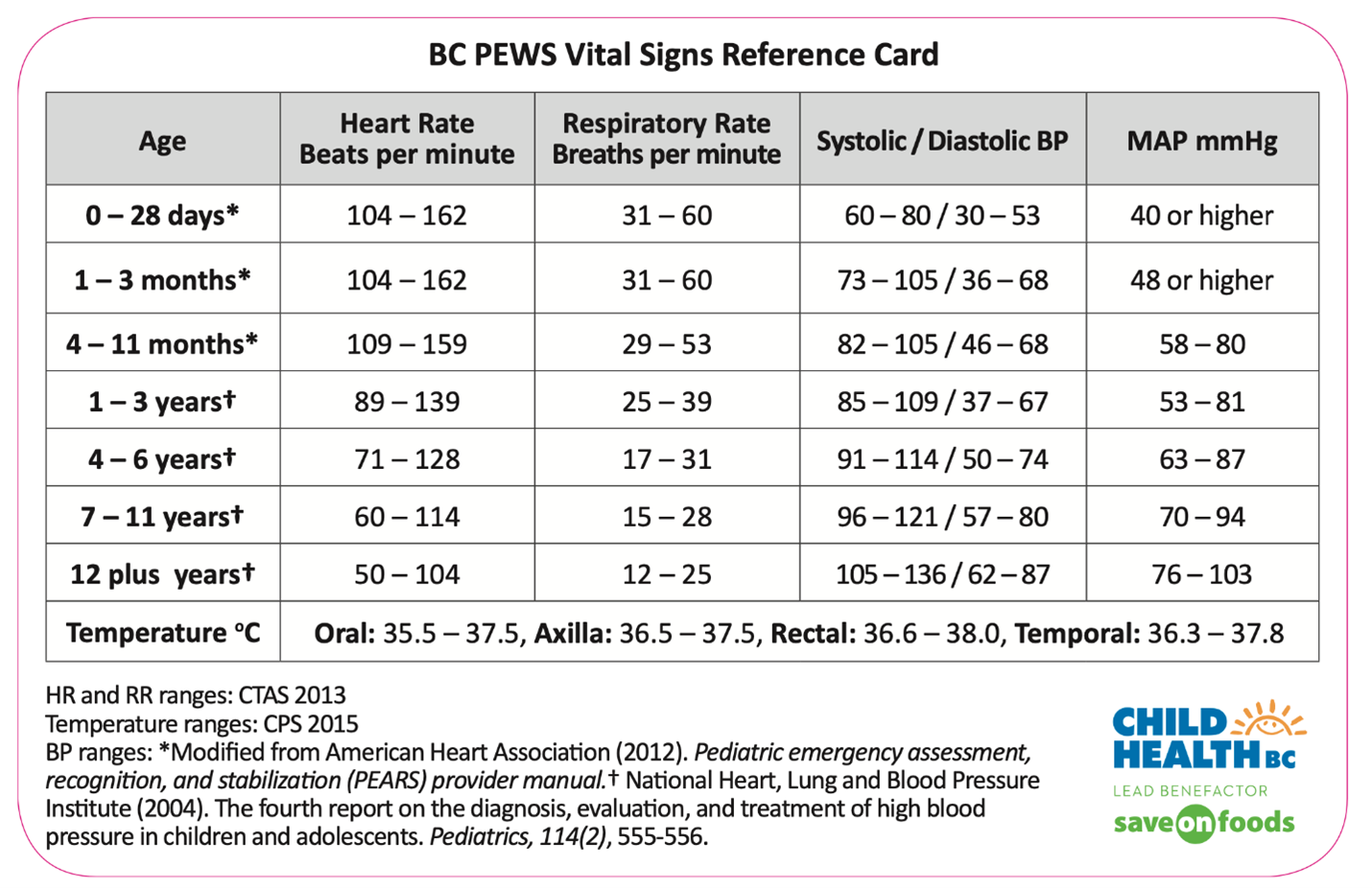
Pediatric Vial Signs:
- Page-For-Age: Is an excellent reference for age and weight based pediatric vital signs and treatments and based off BC Children’s Hospital modified PEWS score.
- Pediatric Early Warning Signs (PEWS): is another resource for pediatric vital signs used by BC Children’s Hospital, found under CPG A02: Patient Assessment.
-